- A. Simone
- Original Article
Short Term Observation: 2008-2015 Activity Report And Data Analysis
- 2/2017-Giugno
- ISSN 2532-1285
- https://doi.org/10.23832/ITJEM.2017.012
- MD Director Short Term observation
- Medical Doctor
- Director of Department of Emergency PErtini Hospital in Roma
Introduction
- To allow an early risk stratification with a reduction of the number of inappropriate hospitalizations
- To determine the risk reduction through early EBM protocols that ensure an effective health care
- To mprove the care process with a reduction of the means used and the consequent cost optimization.
- Chest Pain
- Asthma
- Abdominal pain
- Very old patients with multiple pathologies
- Deep Vein Thrombosis
Matherials and Methods
- A precise diagnostic-therapeutic goal to reach in the 70% of cases with subsequent discharge over 36 hrs
- A limited cure intensity, otherwise hospitalization was ordered
- A proper use of the physician/nurse-patient time
- The clinical record has a dedicated electronic form in the regional system called GIPSE
- All the medical and nursing activities are recorded on the electronic form
- The medical examination is carried out with two laptops (one for the physician and another one for the nurse manager/nurse) linked through wifi connection to the hospital network which allows both of them to assess every variable and issue concerning each patient
- The only paper items, at the moment, are hemogasabalysis and electrocardiogram that are collected in dedicated charts in which just the front page of the record is printed
- After the examination and the valuation, the short term observation unit physician comunicates to the patient the outcome and the decision about discharge or the continuation of the hospitalization. In case of old, fragile and/or disabled patients, families are reached by phone and summoned for an interview
- At the end of the interview with the family and considering the overall family issues, a pathway is activated: discharge; patient return to their recidence by ambulance transport, CAD and ADI activation, transfer to other internal medicine or specialist care structures; hospitalization continuation in other wards inside the same hospital
- Discharge from the STO section has to be seen through over the morning
- The STO form allows to discharge the patient during the examination since notes and prescriptions can be filled through a few steps in the GIPSE form, that can be printed and handed to the patient and the family.
- Admittance in sto for triage color code
- Admittance in sto for diagnosis in the emergency room
- Admittance in sto for pathology (code ICD10)
- Discharged for pathology (code ICD10)
- Hospitalized for pathology
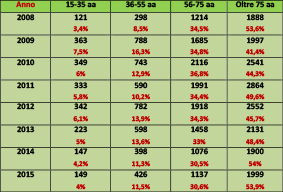
- Hospitalized for age and gender
- Transferred to other structures
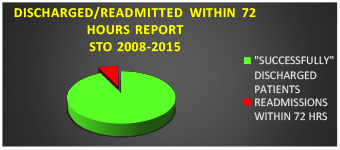
- Readmission within the 72 hours
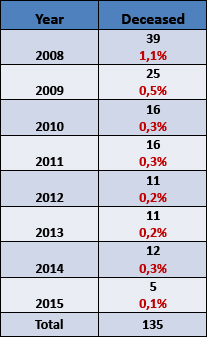
- Deaths
Results
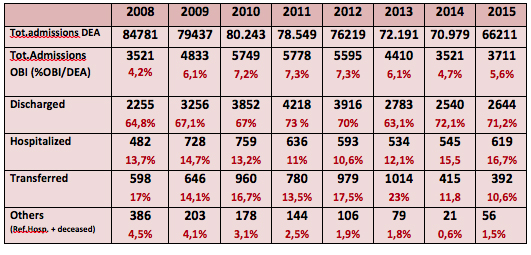
Table 1: Analysis patients for year with a percentage of discharged
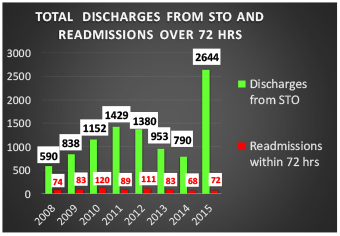
Graphic 1: Total discharges from STO and readmissions over 72 hrs/year
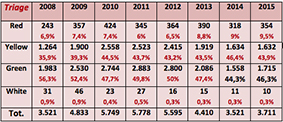
Regarding the priority codes, in the STO section there’s a prevalence of green and yellow codes, with a trend that remained more or less constant over the years.
The hospitalization analysis by age range showed a prevalence of patients over 75 years of age, confirming the role of the STO section in managing the clinical conditions connected to the fragility of old age.
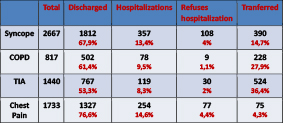
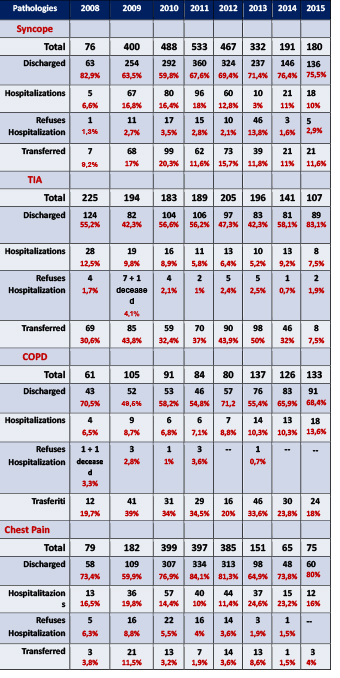
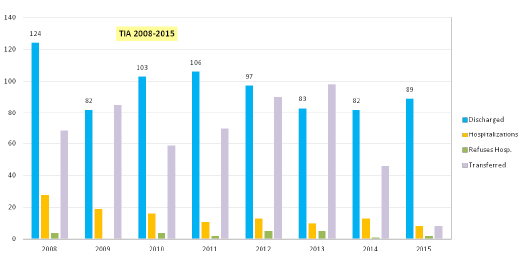
- Transient Ischemic Attack
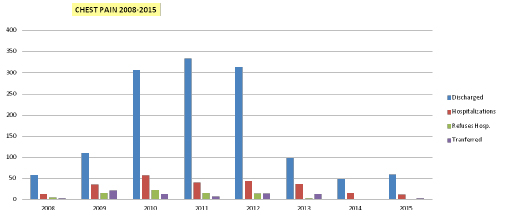
- Chest pain
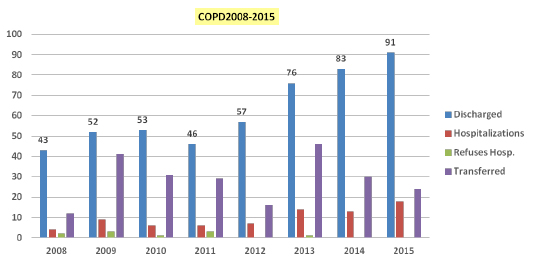
- Acute exacerbation of chronic bronchitis
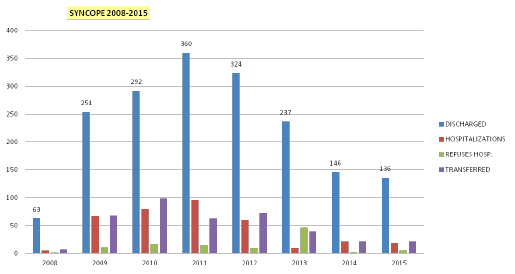
- Syncope
It’s important to point out that over the course of the considered years there was a variation in the users demand that resulted in modifications of the organization of the Emergency Room.
For example the number of admissions in STO with “chest pain” as main symptom decreased with the institution of clinical pathways that allowed the discharge of that category already from the Emergency Room. On the contrary, there was an increase of the admissions in the STO of patients with social fragility and patients over 75 years of age, for an increase of these categories of the population.
Table 7: Analysis of prevailing pathologies
Conclusions
These last few years experience made us grow and encouraged us in the research of an increasingly better appropriateness of the care delivered, paying great attention to our patients’ social and welfare issues. Our experience has identified the main focus of activity dell’OBI in the interview with the patient and his family, a real centerpiece for the management and the appropriateness of both hospital locations on the territory.
to achieve the objective that we set (70% resignations and 30% admissions) was possible in large part thanks to the alignment of all staff behavior, that has formed on field, and daily membership and filed with the method of work.
It is most important for this purpose an increasing integration of the territory with the emergency departments.