- F. Faraldi
- Review
The standing algorithm and triage application in ed: a new approach to identify and classify patients with acute vertigo in different emergency care setting
- 3/2019-Ottobre
- ISSN 2532-1285
- https://doi.org/10.23832/ITJEM.2019.033
F. Diolaiuti1, F. Faraldi1, F. Franchi 1, C. Courtney2, S. Vanni3, R. Pecci4, A. Pavellini4, P. Vannucchi P4, S. Grifoni4, G. Pepe1
1. Emergency Department Versilia Hospital, Azienda USL Toscana Nord Ovest
2. Emergency Department and Stroke Unit, Zaans Medisch Centrum, Noord Holland
3. Emergency Department San Giuseppe Hospital, Empoli, Azienda USL Toscana Centro
4. Emergency Department and Trauma Centre, Azienda Ospedaliero-Universitaria Careggi, Firenze, Italy

Abstract
Acute vertigo is one of the most common causes of access in the emergency department. Healthcare personnel working in ED is not very accurate in diagnosing vertigo. It is useful to include a path and a valid approach for the evaluation of this symptom. The Italian Society of Emergency Medicine and Emergency SIMEU promotes an on the job training based on the “standing” method, a path that uses a diagnostic tool of good reliability and high accuracy in excluding central causes of vertigo. The Mini-Standing is an algorithm applied by triage nursing staff that does not provide a diagnosis but allows a classification of the problem since the patient’s access to ED, allowing better management of available resources and increasing the quality of assistance provided to the patient.
Keywords
Vertigo, standing, triage, emergency, medicine, nurse.
Introduction
Vertigo / unsteadiness is a common symptom which causes 1 to 3 % of presenting on an Emergency Department (ED). Mostly, the aforementioned symptom is caused by a benign cause, such as BVVP or by an inflammation from the inner ear, but it could also be a clear symptom of something worse like a stroke. To be sure that it’s not the worst one, in most of the Italian hospitals (even in international ones) the patient will be subjected to a brain scan (CT) or MRI; if the images show nothing relevant, the patient will be sent to different doctors, suspecting both a neurological and a peripheral cause. The patient will stay hours at the Emergency Department and will live an appropriate called “ vertigo tour”. This causes a long waiting for the patient and often a waste of money for the Hospital. The primary aim of triage is to rapidly identify patients with critical and time-sensitive conditions and to prioritize their care above those who can wait1. In Tuscany, Italy, from 2018 the new organizational model for homogeneous routes in Emergency Room (ER) is underway, since it is emerged the need to guarantee a way of taking charge that defines, from the first contact, the most suitable route for each patient, in order to ensure an effective and fast management of the whole case that accesses the ED. In the new organizational model for homogeneous paths, the input decision-making process integrates assessments of clinical priority and assistance complexity to direct the patient to the appropriate path from the triage and facilitate the flow of patient flows within the ED. At the start of the diagnostic- therapeutic path, the most suitable treatment field is identified based on the patient’s clinical-care characteristics and the potential absorption of resources. Unlike the ED organized by priority code, in the new model the patient is accepted on the basis of his clinical need and the required care complexity. The choice of the path represents the outcome of a combination of several evaluations: “clinical conditions and evolutionary risk”, “absorption of resources”, “assistance needs”. Most of the clinical-care pathways can be traced to three lines of activity with increasing complexity: Line of activities with High complexity, intermediate and Low complexity2. (Figure 1)
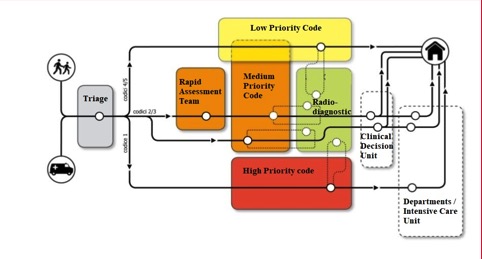
Figure 1.
Redistribution of triage evaluation scores from five to three tiers (from white to green colour, in the past Italian model) was performed to analysis the clinical impact of triage decisions: triage levels 1 and 2 are considered time-sensitive and are roomed immediately, while level 3 patients often wait hours to receive definitive care by emergency physicians, and levels 4 and 5 are cared for in a dedicated area of the ED or with a fast track designation.
Fast Track Designation
The organizational models implemented in the United States, United Kingdom, Canada and Australia, are oriented to the management of cases with less criticality and aim to identify at the time of triage, together with the main problem, the prevalent specialist component to orient the patient’s sending to specific route. These specialized courses (pediatric, gynecological, orthopedic) and any diagnostic facilities constitute the Fast-Track (FT) Area for the management of minor cases according to well-defined therapeutic diagnostic protocols, with a prevalent nursing component. The visit is often decisive of the access of ED. In Italy the different regional models tend to streamline processes avoiding passages without added value. In this sense, the orientation to be privileged is to identify, already from the triage, the criteria for sending direct to the specialist of the path of FT. In the last few years numerous protocols of direct transmission to diagnostic tests have been tested positively before the specialist evaluation. The latter had initially found interpretative difficulties in particular in relation to the request for diagnostic tests. However, it was then clarified that the request can be included as a preordained response in application of protocols shared among the professionals and validated by the company Departments while, in other cases, the prescriptive act can be traced directly to the radiologist specialist. In Tuscany, some FT (Orthopedic, Pediatric, Ophthalmic, Otorhinolaryngologic, Urological, Obstetric-Gynecological and Dermatological) courses have already started with the following organizational solutions: the paths are activated by the triage nurse according to predefined criteria, shared with the competent specialized organizational structures; the clinical responsibility is in charge of the medical specialist, who accesses only the list of patients of that path, closes the case using the application of access management of ED and prints the clinical documentation to be delivered to the patient on headed paper bearing the name of each path and the responsible OU; it is possible to re-enter the patient in the ED path in case of inappropriate sending; the access privileges to specific software, referred to above, and the identification of each path for each patient allow the accurate analysis of FT activity data.
To achieve significant results in the application of FT models it is therefore necessary the preliminary sharing, by the doctors of the different disciplines and nursing staff, and the consequent formalization of company protocols for the fast management of patients who access the ED for minor pathologies. frequent in which there is clear evidence of the clinical problem.
The FT is one of the possible routes launched to the triage for the management of cases with lower criticality – urgency – intensity and is activated in all hospitals in relation to the specialist activities present. The FT is activated by sending to the specialist visit by the triage nurse on the basis of specific protocols active in the garrison (ophthalmology, otolaryngology, orthopaedics, etc.). The specialist, after completing the clinical-care path, provides for the discharge of the patient. The paths of FT differ from the “discharge from ED with sending to the clinic” because: in the FT the path specialist is the first physician to carry out the visit, which is provided, from the temporal point of view, according to the priority assigned to the triage;
in the discharge by sending to the clinic the emergency doctor has already visited the patient, the visit can also be postponed for one or more days. The conclusion of the course does not normally provide for the patient to return to the DP, except in cases where discharge is not possible due to clinical reasons and therefore it is necessary to rely on the emergency doctor.
See & Treat
Minor urgencies, on the other hand, can be managed by ED’s nurse through shared interdisciplinary protocols. This model is called See & Treat (S&T). The S & T is the recommended approach for the management of cases with low intensity of care and diagnostic and organizational complexity that is presented at the ED. The S & T path is activated by the Triage nurse on the basis of validated regional protocols. The patient is taken care of in the S & T area by the nurse with specific training that applies the procedures established by the protocol, solves the patient’s need and, after sharing the case with the doctor, directly realizes the discharge at the completion of the path.
At any time, as the clinical condition changes, the patient can be reinserted in the “traditional” path of ED. In other cases, based on predefined protocols, it can be sent directly to alternative routes with low complexity such as FT. The general protocols of S & T apply in generalist ED, which may also contain indications for the pediatric age range, while in pediatric ED specific protocols of pediatric S & T are developed. The S & T is based on pre-defined medical-nursing protocols that provide inclusion and exclusion criteria for recruitment to individual problems. This path is managed by an adequately trained nurse who operates according to these protocols. In organizing the line of activities with low complexity, the S & T is guaranteed by the presence, at each shift, of at least one certified nurse and by its flexible employment. In ED with a number of annual access exceeding 30,000, or with monthly peaks greater than 2,500, which can be assessed on the basis of seasonal access trends, the presence of a nurse dedicated to S & T activity may be necessary, where the management function operational identify the need.
All nurses with an experience of at least two years in ED (Adult and / or Pediatric depending on the type of ED), and in possession of the certification in Triage, can be trained for the management of the S & T protocols, after evaluation of the attitudes part of the nursing coordinator.
The number of nurses trained is defined in relation to the activity to be performed in each individual ED, so as to ensure the presence of the function in the time slots provided for in relation to the qualitative and quantitative distribution of accesses with a minor code.
The S & T activities are monitored, at least annually, by the nursing coordinator with respect to the predefined quality standards, with individual feedback also for the assessment of the retention of skills. At least every three years a revaluation of the welfare protocols must be carried out in order to verify their topicality, guaranteeing maximum adherence to scientific evidence.
The progressive drafting of new S & T protocols and the updating of existing ones must be carried out with the aim of extending the enlisting case series2.
Ed Triage
The triage, the first moment of reception and the health care of the people who arrive in ED, is a nursery competence aimed to identify the clinical-care priorities through the evaluation of the patients’ clinical conditions, the evolutionary risks and the estimated resource commitment for treatment. The triage defines the order of access to treatment and the start of the appropriate path according to the protocols adopted in ED. The triage nurse manages the waiting time and assigns each patient to the homogeneous path and to the single reference professionals. The waiting time ends when a doctor or nurse out the first activities from the clinical-care path indicated for that patient. The representation of the triage codes provides for an increasing numbering as the priority decreases. Each priority code corresponds to a name, a definition and a maximum waiting time recommended for starting the route2. To avoid unnecessary exams and impatient waiting for patients who suffer vertigo, in 2014 in the Hospital Careggi (Florence) and in 2017 in Versilia (Lucca), first Hospitals in Italy, it has been introduced the STANDING algorithm. This approach represents a line of activity consisting of the set of professional, technological and structural resources already planned for the clinical-care path of patients who present in ER with isolated acute vertigo. Following a few simple steps, this algorithm has shown to lead the patient to a correct pathway and right treatment after suspecting a central or peripheral cause of vertigo. Furthermore, this test can be done by another specialist healthcare professional like an ED doctor or a nurse3.
The Standing Algorithm
The STANDING algorithm (SponTAneous Nystagmus, Direction, head Impulse test, standing) (Figure 2) can be combined in a four-step sequence:
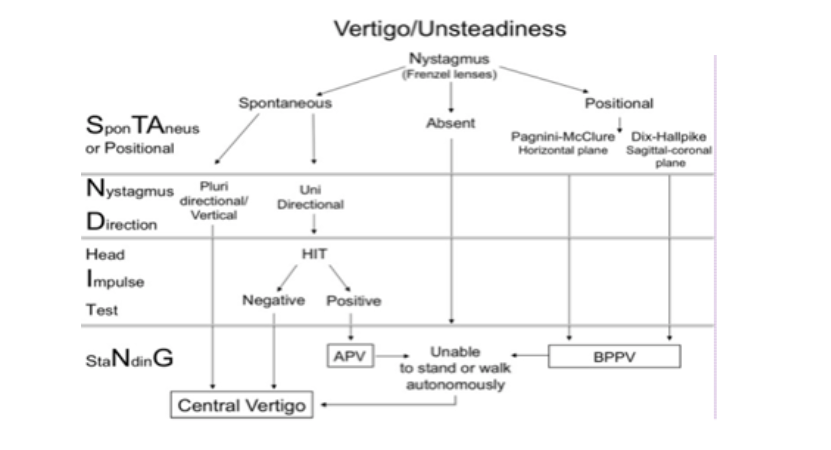
1. Assessment of the presence and of type of nystagmus (Spontaneous, positional, absent);
2. Assessment of nystagmus direction (Nystagmus Direction);
3. Head Impulse Test (HIT);
4. Evaluation of the standing position and gait.
STEP 1 Assessment of the presence and of type of nystagmus (Spontaneous or Positional)
Spontaneous nystagmus
The algorithm starts with the recognition and evaluation of nystagmus. Better evaluation is done with the Frenzel lenses, which gives no prospective to the patient. The patient is in a supine position after at least 5 min of rest, then we start first with the head straight and then the patience has to move his eyes first to the right and then to the left and then up and down. If nystagmus is presented his direction has to be evaluated and classified in horizontal, vertical, torsional or multidirectional nystagmus (Step 2). If there is no nystagmus Pagnini-Mc Clure and Dix-Hallpike will be performed to investigate a positional nystagmus.
Positional nystagmus, Pagnini– MC Clure and Dix Hallpike
Mostly if a patient has a positional nystagmus, he comes to the ED laying on one side, with strong symptomatology of vertigo and nausea; this nystagmus is typical for BPPV where free-floating endolymph particles in the inner ear (otoliths) causes an exaggerate stimulation of the equilibrium receptors. To investigate which canal of the inner ear is interested a clinician has to perform the Pagnini Mc Clure test for the lateral canal and Dix Hallpike for the posterior canal.
Pagnini – Mc Clure. In this test the patient is supine, and the clinician is standing at his head. The patients head is turned 90 degrees first to one side and then to the other. For every side nystagmus shows within one minute. If nystagmus has been noticed, this can be down beating, harder on the sick ear or up beating, harder on the health ear. Dix Hallpike. The patient begins sitting up, and their head is oriented 45 degrees toward the ear that is going to be tested. The clinician stands at extended side and quickly lows the patient to the supine position with his head hyperextended and maintaining the initial rotation of 45 degrees3. If test is positive the nystagmus that we can notice is vertical with a little counter clockwise rotation component on the sick ear side. The patients are always asked to keep his eyes open to evaluate characteristics of nystagmus.
STEP 2 Assessment of Nystagmus Direction
For every position, spontaneous nystagmus has to be evaluated and, if the patient shows nystagmus also in only one of those positions, the test is positive, and it will be classified in:
• horizontal unidirectional (left or right); • multidirectional; • vertical
If the last two types of nystagmus are detected, there is an immediate suspect of a central vertigo and the patient has to be directed to other exams. If the patient has a horizontal nystagmus, the Head Impulse Test (HIT) test will be done. Here, the vestibule-ocular reflex will be tested, whom damage causes this type of nystagmus.
STEP 3 Head Impulse test (HIT)
The patient is seat on the bed side and the clinician hold his head with both hands, in front of him. With a sudden movement the physician turns the patients head, sharp to one side. The patient has to keep his eyes fixed on a spot and if the patient presented a corrective eye movement the test will be positive due to a damage of the VOR on that side. Both patient’s sides had to be done for a correct evaluation. If the patient shows nystagmus in one direction and the Hit is positive for that side, we will conclude that the patient has a problem from the inner ear, and he would be sent to the otolaryngologist. But if no variations have been seen during this test, is has to suspect a central problem and other diagnostic test has to be done.
STEP 4 Evaluation of the standing position and gait (staNdinG).
Standing
The last step of the STANDING algorithm is performed by all patients, in particular those showing neither spontaneous nor positional nystagmus. The patient is asked to stand, and his gait is evaluated, if the patient is unable to stand or walk without assistance, a central cause of vertigo has to be suspected3.
Results
This algorithm has been studied in hospital Careggi ( Tuscany ) and 352 patients have been involved from October 2015 to March 2016. The results that came out where very significant: the accuracy was 88% and it demonstrates high sensitivity (95%) and specificity (87%). With this algorithm the waiting time for the patient was drastically reduced and so the costs made by the ED, avoiding a lot of imaging tests and other unnecessary specialist consults. (Figure 3)
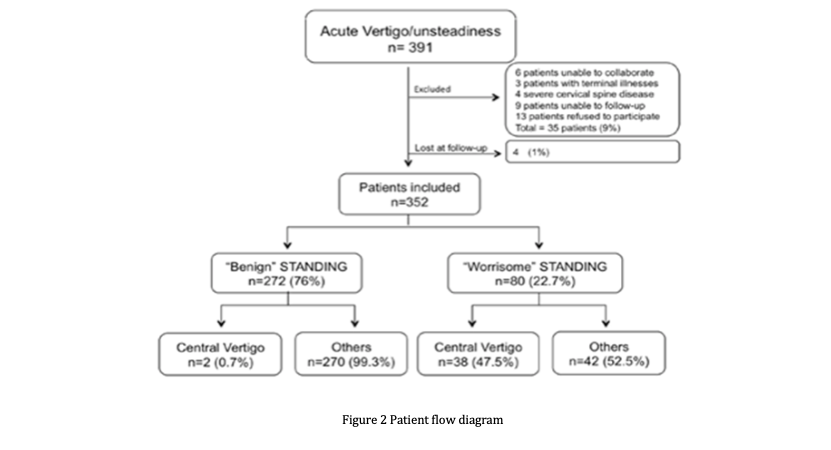
Figure 3. Patient flow diagram
In conclusion, using the STANDING algorithm, non-sub-specialists achieved good reliability and high accuracy in excluding stroke and other threatening causes of vertigo/unsteadiness3.
Triage at the Emergency Department
The STANDING algorithm has been introduced at Versilia Hospital, in Tuscany, in 2017. Only few clinicians have been formed but, until now, only a few doctors are using this test in the Emergency Department. Nowadays, if a patient comes to the ED, a nurse assigns a priority code at the triage and, associated with the ABCD and the suspected cause of the symptoms, the patient will be evaluated by an Emergency doctor in the post-triage. Here he will apply the STANDING algorithm. The use of this algorithm has still to be implemented because not all of the physicians are yet using this latter and patient are still sent immediately to do imaging “because it’s safer”. But what could make the big difference, to safe waiting time in the ED and get a quicker treatment, is to let the nurse perform the algorithm at the first approach with the patient. According to the “Frontiers of neurology” applying the STANDING at the triage, a nurse (or any non-specialist ) could in about five minutes suspect a central or a peripheral cause. (Figure 4)
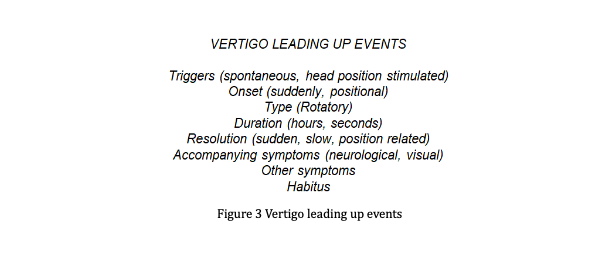
Figure 4. Vertigo leading up events
It has also been created a Mini-STANDING (Figure 5 ) which could be used by nurses at the triage in association with the routine ABCDE and the AMPLE questions.
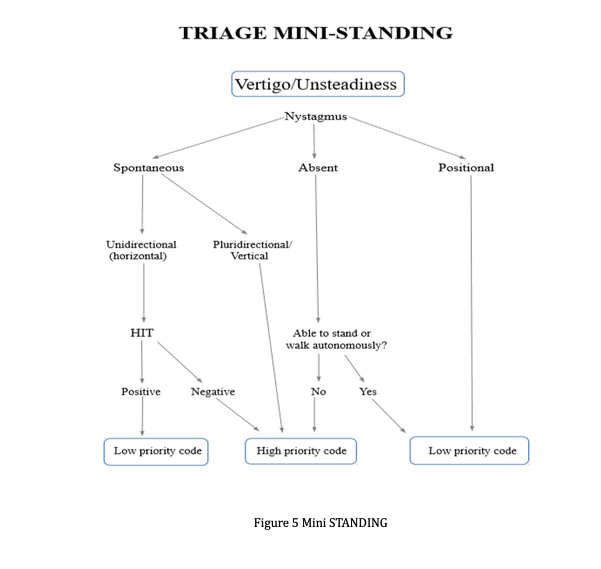
Figure 5. Mini STANDING
After the ABCDE approach gave practical advice on emergency management of unwell patients, a few questions, under the acronym AMPLE, have to be asked to the patient to investigate the cause of his symptoms, in addition to define his health assessment :
A: allergies
M: medications the patient use. Here, eventually, the abuse of some medications could explain the symptoms
P: past illness, history of diseases, operations, hearth diseases, diabetes, high blood pressure…
L: last meal
E: events leading to the injuries, here the nurse has to investigate the events which lead up to the present illness. The questions which help to better investigate the cause and the symptoms are reported on image below.
Suspecting a central cause, the patient will be sent with a high priority code to the ED physician were another diagnostic test will be done. On the contrary, if a peripheral cause is suspected after performing the algorithm, the patient will be sent to a lower priority lane, symptoms will be relieved and BPPV could be simply solved with manoeuvres to reposition the otoliths. If necessary, the patients could also be dismissed through the fast track (fast dismissal to a specialist physician after a quick evaluation in the ED) to a specialist in otology. This first line STANDING approach could make the treatment for vertigo patient faster and it could make the doctors job a little lighter. The STANDING algorithm, because his use has been proved safe even if performed by non- specialized health care professional, should be also performed by nurses at the ED, whom experience and their relevance to protocols would lead to a good management of patients with vertigo. Mini-Standing algorithm performed by a nurse at triage doesn’t give a diagnosis and could be compared to making an ECG on suspected myocardial infarction.
Conclusions
The STANDING algorithm with the phases that include the evaluation of the presence and the type of nistagm and the evaluation of its direction, the test of the pulsations and the evaluation of the standing position and the gait of the patient, is therefore a good evaluation method if used by medical and/or nursing staff.
The main implications of the insertion of the algorithm in cases of emergency and acceptance can therefore be described in a faster and more reliable management of the provision of health services provided, ultimately leading to an increasingly adequate management of resources.
References
- Iserson KV, Moskop JC. Triage in medicine, part I: concept, history, and types. Ann Emerg Med. 2007;49(3):275–281. doi: 10.1016/j.annemergmed.2006.05.019.
- Modello organizzativo per percorsi omogenei in Pronto Soccorso. Linee di indirizzo. Delibera GRT N 806 del 24-07-2017
- Vanni S., Pecci R., Wadlow J.A., Nazerian P., Santimone R., Pepe G., Moretti M., Pavellini A., Caviglioli C., Casula C., Bigiarini S., Vannucchi P., Grifoni S. 2017 “Frontiers in Neurology, Differential Diagnosis of Vertigo in the Emergency Department: a prospective validation Study of the STANDING algorithm. “vol. 8, article 590:2
Abbreviations
stanDinG: Spontaneous Nystagmus, Direction, head Impulse test, standing; ED: emergency Department; FT: fast track; S&T: See & Treat; BVVP: benign positional paroxysmal vertigo; CT: Computer Tomography; MRI: magnetic resonance imaging; HIT: Head Impulse Test; VOR: Vestibule-ocular reflex; AMPLE: Allergies, Medications, Past Illnesses, Last meal, Events; ABCDE: Airway, Breath, Circulation, Disability, Exposure.

