- Sozio Emanuela
- Original Article
Early detection of severe cases due to sepsis in Emergency Department in in the era of New Diagnostic Criteria: preliminary data from an Italian “real life” study
- 2/2019-giugno
- ISSN 2532-1285
- https://doi.org/10.23832/ITJEM.2019.017
Sozio Emanuela1, Tarabori Serena2, Bertolino Giacomo3, Carfagna Fabio 4, Novelli Francesca2, Di Paco Irene 1, Tascini Carlo5, Santini Massimo6, Ghiadoni Lorenzo2, Bertini Alessio1
-
Emergency Department , North-West District, Tuscany Health Care, Spedali Riuniti Livorno, Leghorn, Italy
-
Emergency Medicine Unit, Nuovo Santa Chiara University Hospital, Azienda Ospedaliera Universitaria Pisana, Pisa, Italy
-
Department of Public Health, Clinical and Molecular Medicine, Università degli studi di Cagliari, Italy
-
Azienda Ospedaliero Universitaria Maggiore della Carità, Novara, Italy
-
First Division of Infectious Diseases, Cotugno Hospital, Azienda Ospedaliera dei Colli, Naples, Italy
- Emergency Department, Nuovo Santa Chiara University Hospital, Azienda Ospedaliera Universitaria Pisana, Pisa, Italy
Abstract
Keywords
Sepsis-3; Sepsis; Septic shock; qSOFA; MEWS
Abbreviations
Introduction
Early recognition is a key point of the entire management of sepsis because it allows a timely treatment and this improves survival1, 2. Worldwide estimated incidence is 270 cases per 100,000 inhabitants/year and the mortality rate ranges between 20 and 40%3.
Methods
This real-life prospective study enrolled 349 patients admitted to the ED of Pisa Hospital from 1 March 2017 to 31 May 2018 with diagnosis of infection with or without clinical criteria of sepsis or septic shock, according to the new definitions of sepsis and septic shock (Sepsis -3). Cases were identified through the ICD-9-CM codes and the ED discharge diagnosis of sepsis, severe sepsis or septic shock. The definition was different because the new one had not been introduced in (the) daily clinical practice yet.
Results
|
|
Overall population |
Infections without sepsis or septic shock criteria |
Sepsis or septic shock criteria |
p-value |
|
(n = 349) |
(n = 54) |
(n = 295) |
||
|
Age |
80.0 (71.0 – 87.0) |
76.0 (65.0 – 85.0) |
81.0 (72.0 – 87.0) |
p = 0.023 |
|
Male sex |
211 (60%) |
36 (67%) |
175 (59%) |
p = 0.388 |
|
Diabetes |
87 (25%) |
17 (31%) |
70 (24%) |
p = 0.298 |
|
CCI |
2.0 (1.0 – 4.0) |
3.0 (2.0 – 5.0) |
2.0 (1.0 – 4.0) |
p = 0.015 |
|
qSOFA |
86/316 (27%) |
2/52 (4%) |
84/264 (32%) |
p < 0.001 |
|
SOFA score |
4.0 (3.0 – 6.0) |
3.0 (1.0 – 4.0) |
4.0 (3.0 – 6.0) |
p < 0.001 |
|
GCS |
15.0 (13.0 – 15.0) |
15.0 (15.0 – 15.0) |
15.0 (11.0 – 15.0) |
p < 0.001 |
|
MEWS |
2.0 (1.0 – 4.0) |
1.0 (0.0 – 2.0) |
3.0 (1.0 – 5.0) |
p < 0.001 |
|
Shock Index |
0.8 (0.7 – 1.1) |
0.7 (0.6 – 0.8) |
0.8 (0.7 – 1.1) |
p = 0.001 |
|
End-stage renal failure |
11 (3%) |
3 (6%) |
8 (3%) |
p = 0.396 |
|
Chronic Liver diseases |
19 (5%) |
5 (9%) |
14 (5%) |
p = 0.309 |
|
COPD |
44 (13%) |
13 (24%) |
31 (11%) |
p = 0.011 |
|
Tumors |
68 (19%) |
18 (33%) |
50 (17%) |
p = 0.009 |
|
Immunodepression / immunosuppresion |
35 (10%) |
8 (15%) |
27 (9%) |
p = 0.304 |
|
Previous surgery |
32 (9%) |
6 (11%) |
26 (9%) |
p = 0.778 |
|
Previous trauma exposure |
22 (6%) |
3 (6%) |
19 (6%) |
p = 1.000 |
|
Previous antimicrobial treatments |
126/343 (37%) |
22/53 (42%) |
104/290 (36%) |
p = 0.529 |
|
Corticosteroid treatments |
62 (18%) |
12 (22%) |
50 (17%) |
p = 0.460 |
|
Prostheses |
57 (16%) |
13 (24%) |
44 (15%) |
p = 0.141 |
|
CVC |
38 (11%) |
5 (9%) |
33 (11%) |
p = 0.857 |
|
Bladder Catheter |
57 (16.3%) |
5 (9.3%) |
52 (17.8%) |
p = 0.120 |
|
SIRS criteria |
233 (67%) |
30 (56%) |
203 (69%) |
p = 0.081 |
|
Hospitalization |
331 (95%) |
52 (96%) |
279 (95%) |
p = 0.849 |
|
ICU |
30 (9%) |
2 (4%) |
28 (9%) |
p = 0.258 |
|
Overall mortality |
76 (22%) |
4 (7%) |
72 (24%) |
p = 0.009 |
|
In-emergency department mortality |
14 (4%) |
0 (0%) |
14 (5%) |
p = 0.126 |
|
In-Hospital mortality |
62/331 (19%) |
4/52 (8%) |
58/279 (21%) |
p = 0.042 |
|
Discharge a home |
4 (1%) |
2 (4%) |
2 (1%) |
p = 0.130 |
|
Length of hospital stay (days) |
7.0 (4.0 – 10.0) |
6.5 (5.0 – 12.0) |
7.0 (4.0 – 10.0) |
p = 0.213 |
|
MAP |
132.7 (113.3 – 156.7) |
139.7 (122.7 – 162.0) |
128.3 (111.7 – 156.7) |
p = 0.041 |
|
Hypotension |
101/313 (32%) |
7/50 (14%) |
94/263 (36%) |
p = 0.004 |
|
Body Temperature (°C) |
37.6 (36.7 – 38.5) |
37.6 (36.5 – 38.1) |
37.6 (36.7 – 38.5) |
p = 0.285 |
|
WBC ᴧ103 |
13.9 (9.4 – 20.8) |
13.9 (10.0 – 20.1) |
13.8 (9.3 – 21.1) |
p = 0.865 |
|
Platelets ᴧ106 |
190.0 (126.0 – 276.0) |
217.0 (170.0 – 289.0) |
184.0 (123.0 – 273.0) |
p = 0.058 |
|
Plasmatic creatinine value (mg/dl) |
1.4 (0.9 – 2.2) |
1.2 (0.9 – 2.1) |
1.4 (1.0 – 2.3) |
p = 0.130 |
|
Lactate value (mmol/l) |
1.8 (1.1 – 3.3) |
1.0 (0.8 – 1.2) |
2.1 (1.2 – 3.6) |
p < 0.001 |
|
PCT value (pg/ml) |
2.3 (0.6 – 11.2) |
1.0 (0.4 – 4.4) |
2.7 (0.7 – 12.4) |
p = 0.010 |
|
Bilirubin value (mg/dl) |
0.6 (0.4 – 1.1) |
0.5 (0.3 – 0.7) |
0.7 (0.4 – 1.2) |
p = 0.006 |
|
Blood cultures |
128/314 (41%) |
22/52 (42%) |
106/262 (40%) |
p = 0.925 |
|
Intravenous fluids |
303 (87%) |
46 (85%) |
257 (87%) |
p = 0.867 |
|
Antibiotic therapy BEFORE sampling blood cultures |
89/126 (71%) |
17/23 (74%) |
72/103 (70%) |
p = 0.898 |
|
Empiric antibiotic therapy |
249/343 (73%) |
38/53 (72%) |
211/290 (73%) |
p = 1.000 |
|
Qualitative variables |
Survivors (n=273) |
Overall mortality (n=76) |
*p value chi square or fisherF’s test |
||
|
n. |
% |
n. |
% |
||
|
Male Sex |
169 |
61.9% |
42 |
55.3% |
0.295 |
|
End-stage renal failure |
9 |
3.3% |
2 |
2.6% |
1.000 |
|
Cardiovascular diseases |
125 |
45.8% |
42 |
55.3% |
0.144 |
|
COPD |
31 |
11.4% |
13 |
17.1% |
0.182 |
|
Diabetes |
69 |
25.3% |
18 |
23.7% |
0.777 |
|
Chronic Liver diseases |
17 |
6.2% |
2 |
2.6% |
0.389 |
|
Immunodepression/ immunosuppression |
26 |
9.5% |
9 |
11.8% |
0.552 |
|
Tumors |
59 |
21.6% |
9 |
11.8% |
0.057 |
|
Previous Corticosteroid treatments |
43 |
15.8% |
19 |
25.0% |
0.062 |
|
Previous trauma exposure |
18 |
6.6% |
4 |
5.3% |
0.795 |
|
Previous surgery |
25 |
9.2% |
7 |
9.2% |
0.989 |
|
CVC |
28 |
10.3% |
10 |
13.2% |
0.473 |
|
Bladder Catheter |
41 |
15.0% |
16 |
21.1% |
0.208 |
|
Prostheses |
49 |
17.9% |
8 |
10.5% |
0.122 |
|
Altered mental status |
61 |
22.3% |
43 |
56.6% |
<0.001 |
|
Hypotension |
67 |
27.6% |
34 |
48.6% |
0.001 |
|
PAM <=70 |
4 |
1.6% |
2 |
2.9% |
0.619 |
|
Hypothermia or Hyperthermia |
97 |
39.0% |
14 |
22.2% |
0.013 |
|
Lactate > 1.8 mmol/L |
118 |
43.7% |
62 |
83.8% |
<0.001 |
|
Leukocytosis or leukopenia |
177 |
65.3% |
54 |
73.0% |
0.214 |
|
PCT ≥ 0.5 pg/ml |
202 |
76.8% |
63 |
88.7% |
0.028 |
|
Creatinine ≥ 1.2 mg/dl |
153 |
56.5% |
54 |
74.0% |
0.007 |
|
Bilirubin ≥ 1.2 mg/dl |
34 |
18.6% |
15 |
32.6% |
0.038 |
|
PLT ≤ ᴧ106 |
97 |
35.8% |
25 |
33.8% |
0.749 |
|
qSOFA criteria |
48 |
19.3% |
38 |
56.7% |
<0.001 |
|
SIRS criteria |
176 |
64.5% |
57 |
75.0% |
0.085 |
|
MEWS ≥ 5 |
49 |
17.9% |
35 |
46.1% |
<0.001 |
|
Shock index ≥ 0.7 |
162 |
67.8% |
56 |
81.2% |
0.031 |
|
Quantitative variables |
Survived |
Dead |
*p value Mann-Whitney Test |
||
|
Median |
25-75 Percentile |
Median |
25-75 Percentile |
||
|
Age |
79.0 |
[70 – 86] |
84.0 |
[73.5 – 90] |
0.013 |
|
CCI |
2.0 |
[1 – 4] |
3.0 |
[1 – 4] |
0.366 |
|
GCS |
15.0 |
[14 – 15] |
10.5 |
[6 – 15] |
<0.001 |
|
MAP |
136.67 |
[115 – 160] |
120.00 |
[103 – 140] |
0.001 |
|
Body Temperature (°C) |
37.8 |
[36.8 – 38.5] |
37.0 |
[36.0 – 38] |
0.001 |
|
Lactate value (mmol/l) |
1.6 |
[1.0 – 2.7] |
3.9 |
[2.0 – 6.6] |
<0.001 |
|
WBC ᴧ103 |
13.49 |
[9.27 – 19.75] |
15.91 |
[9.43 – 24.92] |
0.072 |
|
PCT (pg/ml) |
2.0 |
[0.5 – 10.6] |
3.0 |
[1.2 – 16.8] |
0.038 |
|
Plasmatic creatinine (mg/dl) |
1.3 |
[0.9 – 1.9] |
2.0 |
[1.1 – 3.5] |
<0.001 |
|
Bilirubin (mg/dl) |
0.59 |
[0.38 – 1.00] |
0.96 |
[0.47 – 1.60] |
0.005 |
|
Platelets ᴧ106 |
186.0 |
[128.0- 274.0] |
195.5 |
[109 – 292] |
0.942 |
|
SOFA SCORE |
4.0 |
[3.0 – 5.0] |
6.0 |
[4.0 – 9.0] |
<0.001 |
|
MEWS |
2.0 |
[1.0 – 4.0] |
4.0 |
[2.5 – 6.0] |
<0.001 |
|
Shock index |
0.77 |
[0.65 – 0.98] |
0.98 |
[0.77 – 1.29] |
<0.001 |
|
Variables |
OR |
CI 95% |
p value |
|
Male sex |
0.760 |
0.455 – 1.271 |
0.296 |
|
Age |
1.026 |
1.002 – 1.050 |
0.031 |
|
End-stage renal failure |
0.793 |
0.168 – 3.749 |
0.770 |
|
Cardiovascular diseases |
1.463 |
0.877 – 2.438 |
0.145 |
|
COPD |
1.611 |
0.796 – 3.258 |
0.185 |
|
Diabetes |
0.918 |
0.506 – 1.664 |
0.777 |
|
Chronic Liver diseases |
0.407 |
0.092 – 1.802 |
0.236 |
|
Immunodepression / immunosuppression |
1.276 |
0.571 – 2.853 |
0.553 |
|
Tumors |
0.487 |
0.229 – 1.035 |
0.061 |
|
Previous Corticosteroid treatments |
1.783 |
0.966 – 3.291 |
0.064 |
|
Previous trauma exposure |
0.787 |
0.258 – 2.399 |
0.674 |
|
Previous surgery |
1.006 |
0.418 – 2.425 |
0.989 |
|
CVC |
1.326 |
0.613 – 2.868 |
0.474 |
|
Bladder catheter |
1.509 |
0.793 – 2.872 |
0.210 |
|
Prostheses |
0.538 |
0.243 – 1.191 |
0.126 |
|
Hypotension |
2.481 |
1.436 – 4.286 |
0.001 |
|
Hypothermia or Hyperthermia |
0.448 |
0.235 – 0.854 |
0.015 |
|
Leukocytosis or leukopenia |
1.434 |
0.81 – 2.537 |
0.216 |
|
qSOFA criteria |
5.487 |
3.082 – 9.769 |
<0.001 |
|
SIRS criteria |
1.653 |
0.930 – 2.939 |
0.087 |
|
CCI |
0.998 |
0.895 – 1.113 |
0.968 |
|
SOFA score |
1.467 |
1.316 – 1.636 |
<0.001 |
|
GCS |
0.804 |
0.753 – 0.858 |
<0.001 |
|
MAP |
0.986 |
0.977 – 0.995 |
0.002 |
|
Body Temperature |
0.660 |
0.517 – 0.844 |
0.001 |
|
Lactate value |
1.364 |
1.224 – 1.519 |
<0.001 |
|
WBC |
1.036 |
1.011 – 1.062 |
0.005 |
|
PCT |
1.005 |
0.996 – 1.014 |
0.310 |
|
Creatinine value |
1.325 |
1.14 – 1.541 |
<0.001 |
|
Bilirubin value |
1.433 |
1.105 – 1.858 |
0.007 |
|
Platelets |
1.000 |
0.998 – 1.002 |
0.919 |
|
MEWS |
1.333 |
1.205 – 1.475 |
<0.001 |
|
Shock index |
6.582 |
2.793 – 15.514 |
<0.001 |
Discussion and Conclusion
Conclusions
Sepsis is of great clinical importance, being responsible for more than one third of all hospital admissions, and it is associated with a large economic burden on healthcare. The Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3) reviewed and updated sepsis definitions. Sepsis is now defined as a “life-threatening organ dysfunction caused by a dysregulated host response to infection”; organ dysfunction is defined as an increase in SOFA score ≥ 2 but SOFA requires laboratory values which may not be rapidly available. qSOFA was developed to provide an abbreviated version that can easily be performed at the bedside by the non-specialist but the main utility of qSOFA appears to be for the characterization of patients with suspected or known infection, in whom sepsis should be considered, who are at a higher risk of developing a poor outcome, and who may benefit from more frequent observations and targeted interventions.
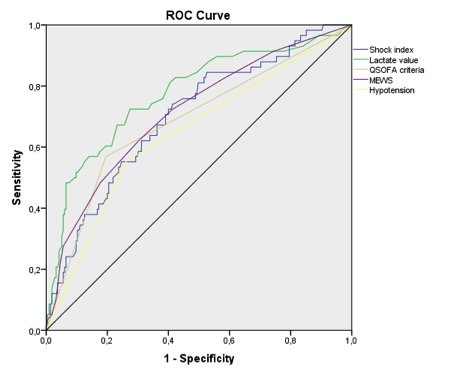
Although all clinical tools used for early diagnosis of triage in ED were sub-optimal, our preliminary analysis showed that lactates value and the use of clinical tools in ED such as EWS (in our case the MEWS) or more simply the shock index, could be used in the triage phase to identify patients at risk of poor prognosis due to sepsis or septic shock. Using these tools as “red flags”, an immediate management could be carried out, after a “few minutes” evaluation during triage phases.
References
-
Dellinger RP, Levy MM, Rhodes A, et al. Surviving Sepsis Campaign: International Guidelines for Management of Severe Sepsis and Septic Shock 2012. Intensive Care Medicine 2013; 39(2):165-228; Critical Care Medicine 2013; 41:580-637
-
Geoffrey E, Hayden MD, Rachel E, et al. Triage sepsis alert and sepsis protocol lower times to fluids and antibiotics in the ED. The American Journal of Emergency Medicine 2016; 34(1):1–9
-
Fleischmann C, Scherag A, Adhikari NKJ, et al. Assessment of Global Incidence and Mortality of Hospital-treated Sepsis. Current Estimates and Limitations. Am J Respir Crit Care Med 2016; 193(3): 259–272
-
Singer M, Deutschman CS, Seymour CW, et al. The Third International Consensus Definition for Sepsis and Septic Shock (Sepsis-3). Jama 2016; 315 (8): 801-810
-
Calci M, Ruggiano G, Causin F et al. Simeu Consensus Conference on management of sepsis and septic shock in Emergency Department: preliminary survey results. ITJEM 2018; n°1
-
Singer AJ, Ng J, Thode HC, et al. Quick SOFA Scores predict mortality in adult emergency department patients with and without suspected infection. Ann Emerg Med 2017; 69(4):475-479
-
Freund Y, Lemachatti N, Krastinova E, et al. Prognostic Accuracy of Sepsis-3 Criteria for In-Hospital Mortality Among Patients With Suspected Infection Presenting to the Emergency Department. JAMA 2017; 317(3):301-308
-
Serafim R, Gomes JA, Salluh J, et al. A Comparison of the Quick-SOFA and Systemic Inflammatory Response Syndrome Criteria for the Diagnosis of Sepsis and Prediction of Mortality: A Systematic Review and Meta-Analysis. Chest 2018; 153(3):646-655
-
Percorso Sepsi. Gestione della Sepsi e dello Shock Settico, Identificazione e Trattamento – Percorso Diagnostico Terapeutico Assistenziale (PDTA). Regione Toscana, Aprile 2016, Delibera n.752 del 10-07-2017 -Allegato A – PROGRAMMA REGIONALE DI LOTTA ALLA SEPSI
-
Bassetti M, Calci M, Cappello Dario, et al. La sepsi: riconoscimento precoce in Pronto Soccorso e gestione della fase iniziale nell’adulto. Direzione centrale salute, integrazione socio-sanitaria, politiche sociali e famiglia Regione Friuli Venezia Giulia 2017.
-
Rivers EP, Nguyen HB, Havstad S, et al. Early Goal-Directed Therapy in the Treatment of Severe Sepsis and Septic Shock. N Engl J Med 2001; 345:1368-1377
-
Osborn TM, Nguyen HB, Rivers EP. Emergency Medicine and the Surviving Sepsis Campaign: An International Approach to Managing Severe Sepsis and Septic Shock. Ann Emerg Med 2005; 46(3):228-231
-
Daniels R, Nutbeam T, McNamara G, et al. The sepsis six and the severe sepsis resuscitation bundle: a prospective observational cohort study. Emerg Med J2011; 28(6):507-12
-
Ferrer R, Martin-Loeches I, Phillips G, et al. Empiric Antibiotic Treatment Reduces Mortality in Severe Sepsis and Septic Shock From the First Hour: Results From a Guideline-Based Performance Improvement Program. Crit Care Med 2014; 42(8):1749-1755
-
Rhodes A, Evans LE, Alhazzani W, et al. Surviving Sepsis Campaign: International Guidelines for Management of Sepsis and Septic Shock: 2016. Intensive Care Medicine 2017;43(3):304-377; Critical Care Medicine 2017; 45(3):486-552
-
Zadroga R, Williams DN, Gottschall R, et al. Comparison of 2 Blood Culture Media Shows Significant Differences in Bacterial Recovery for Patients on Antimicrobial Therapy. Clin Infect Dis 2013; 56(6):790-797
-
De Sousa AG, Fernandes Junior CJ, Santos GPD, et al. The impact of each action in the Surviving Sepsis Campaign measures on hospital mortality of patients with severe sepsis/septic shock. Einstein 2008; 6(3):323-327
-
Kumar A, Ellis P, Arabi Y, et al. Initiation of Inappropriate Antimicrobial Therapy Results in a Fivefold Reduction of Survival in Human Septic Shock. Chest 2009; 136(5):1237-1248
-
Gaieski DF, Mikkelsen ME, Band RA, et al. Impact of time to antibiotics on survival in patients with severe sepsis or septic shock in whom early goal-directed therapy was initiated in the emergency department. Crit Care Med 2010; 38(4):1045-1053
-
Subbe CP, Kruger M, Rutherford P, et al. Validation of a modified Early Warning Score in medical admissions. QJM 2001; 94(10):521-526
-
Singer AJ, Taylor M, Domingo A, et al. Diagnostic characteristics of a Clinical Screening Tool in Combination With Measuring Bedside Lactate Level in Emergency Department Patients With Suspected Sepsis. Acad Emerg Med 2014; 21(8):853-857
-
Churpek MM, Snyder A, Han X, et al. Quick Sepsis-related Organ Failure Assessment, Systemic Inflammatory Response Syndrome, and Early Warning Scores for Detecting Clinical Deterioration in Infected Patients outside the Intensive Care Unit. Am J Respir Crit Care Med 2017; 195(7):906-911
-
Gordo VF, Molina R. Evolución a la detección precoz de gravedad. ¿Hacia dónde vamos?. Med Intensiva 2017; 42(1):47–49
-
Abbott TEF, Vaid N, Ip D, et al. A single-centre observational cohort study of admission National Early Warning Score (NEWS). Resuscitation 2015; 92:89–93
-
Corfield AR, Lees F, Zealley I, et al. Utility of a single early warning score in patients with sepsis in the emergency department. Emerg Med J 2014; 31(6):482–487

