- Garramone A.
- Original Article
High flow nasal cannula in acute respiratory failure: emergency medicine experience
- 1/2019-Febbraio
- ISSN 2532-1285
- https://doi.org/10.23832/ITJEM.2019.008
Garramone A.°, Iaccarino C.*, Giacopelli G.*, Fante E.*, Bresciani E.*, Palange P.§
° Azienda Ospedaliera Regionale San Carlo Potenza
* Emergency Department, Policlinico Umberto I, Rome
§ Internal Medicine and Respiratory Disfunction, Policlinico Umberto I, Rome
Introduction
Acute respiratory failure (ARF) is one of the major causes of access to Emergency Department in Italy.
Oxygen therapy is the main treatment and is traditionally delivered through different devices (i.e. oronasal masks and nasal cannulas) that can provide a low or high oxygen flow depending on the patient’s needs.
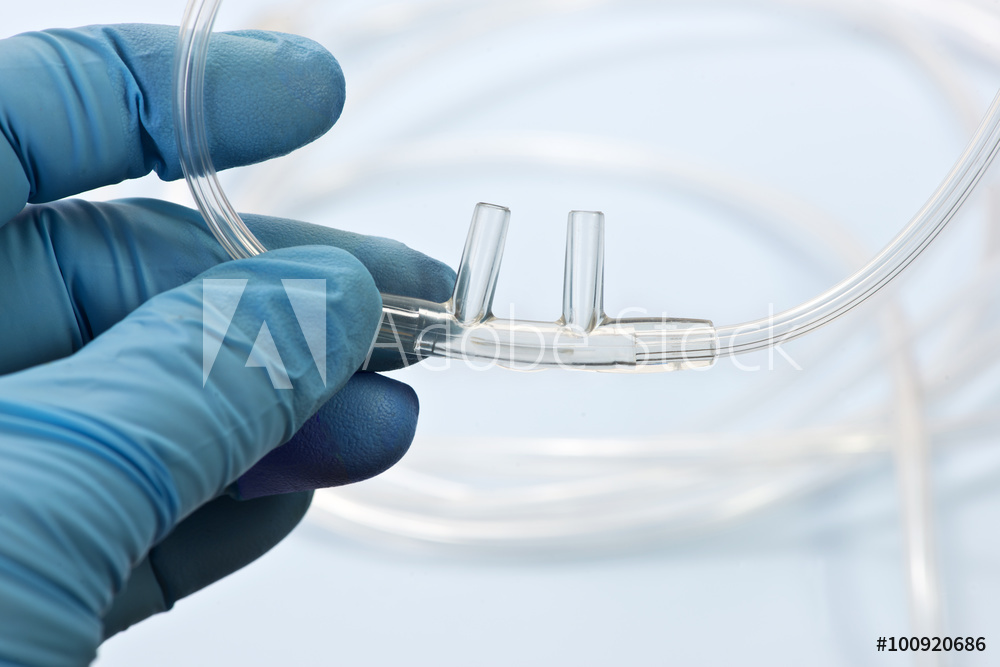
Over the last few years a growing interest has been spreading towards a new technique which grants a high flow of heated and humidified oxygen. Traditionally this treatment is delivered through nasal silicone tubes, not occluding the nostrils, known as High Flow Nasal Cannula (HFNC) (see Figure 1).
Oxygen therapy is the main treatment and is traditionally delivered through different devices (i.e. oronasal masks and nasal cannulas) that can provide a low or high oxygen flow depending on the patient’s needs.
Over the last few years a growing interest has been spreading towards a new technique which grants a high flow of heated and humidified oxygen. Traditionally this treatment is delivered through nasal silicone tubes, not occluding the nostrils, known as High Flow Nasal Cannula (HFNC) (see Figure 1).
Figure 1. System for High Flow Nasal Cannula
Oxygen therapy with HFNC allows to deliver a flow of heated and humidified air with a constant FiO2 that can vary from 21% to 60% depending on the degree of hypoxemia of the patient. The flow of deliverable air ranges from 10 to 60 liters/minute, even if in the adult patient it is preferable to set a minimum flow of 40 liters/minute. The temperature can be set at 31, 34 or 37 degrees centigrade. A peculiar feature is to provide a totally humidified oxygen mixture: at 37 °C there is a content of 44 mg of H2O per liter, which warrants a 100% relative humidity.
In Pediatrics there is a well-established experience regarding the use of HFNC, which have significantly reduced the rate of orotracheal intubation in infants recovered in NICU affected by acute respiratory failure caused from bronchiolitis or other respiratory distresses. For this reason and the growing potential, they also diffuse in Pediatric Emergency Departments.
Even if clinical experiences concerning the treatment of acute respiratory failure in adults using HFNC, are relatively minor compared to Pediatrics’, nevertheless in the last years the Scientific Community has been very interested to this topic and many works about were produced.
Materials and methods
The work is a prospective observational study that aims to investigate the efficacy of high-oxygen therapy flow through HFNC in the setting of Emergency Medicine. This took place in a period from July 2017 to June 2018 in the Emergency Department and in the Emergency Medicine Ward of the University Hospital Umberto I of Rome.
The inclusion criteria were: age > 18 years; presence at the arterial gas analysis of acute respiratory failure (PaO2< 60 mmHg and/or PaO2/FiO2ratio <300). The exclusion criteria were: hemodynamic instability; immediate need for orotracheal intubation.
The patients thus recruited underwent high flow oxygen therapy through the AIRVO2 device of Fisher & Paykel with a flow ranging from 40 to 60 liters per minute and a FiO2variable between 24% and 70%. Operators adjusted FiO2and flow to achieve SpO2≥ 94% for type I ARF and SpO2from 88% to 92% for type II one.
During our observation, frequent arterial gas analysis were performed: before starting the HFNC, at 12, 24, 48 and 72 hours from the start of the treatment and at the suspension.
Other blood and radiological tests performed in the ED together with the remote pathological anamnesis, were also collected.
The primary objective of the study was to verify whether oxygen-therapy with HFNC was able to determine a significant improvement of respiratory failure and respiratory distress using blood gas analysis (reaching an improvement of respiratory values) and clinical criteria (RR reduction). The secondary objective was to identify possible groups of diseases in which HFNC could have a particular effectiveness. The degree of comfort and compliance felt by patients and the occurrence of any complications were also assessed.
The inclusion criteria were: age > 18 years; presence at the arterial gas analysis of acute respiratory failure (PaO2< 60 mmHg and/or PaO2/FiO2ratio <300). The exclusion criteria were: hemodynamic instability; immediate need for orotracheal intubation.
The patients thus recruited underwent high flow oxygen therapy through the AIRVO2 device of Fisher & Paykel with a flow ranging from 40 to 60 liters per minute and a FiO2variable between 24% and 70%. Operators adjusted FiO2and flow to achieve SpO2≥ 94% for type I ARF and SpO2from 88% to 92% for type II one.
During our observation, frequent arterial gas analysis were performed: before starting the HFNC, at 12, 24, 48 and 72 hours from the start of the treatment and at the suspension.
Other blood and radiological tests performed in the ED together with the remote pathological anamnesis, were also collected.
The primary objective of the study was to verify whether oxygen-therapy with HFNC was able to determine a significant improvement of respiratory failure and respiratory distress using blood gas analysis (reaching an improvement of respiratory values) and clinical criteria (RR reduction). The secondary objective was to identify possible groups of diseases in which HFNC could have a particular effectiveness. The degree of comfort and compliance felt by patients and the occurrence of any complications were also assessed.
Statistical analysis
For the statistical analysis of the collected data, Med Calc Ver. 18.5 software was used for the Windows 10 operating system. The statistical distribution of the values examined through the “χ2 test” was analyzed first.
With the exception of the “pH” which revealed a parametric distribution, all the other analytes examined were characterized instead by a non-parametric distribution.
The statistical significance of the both values were respectively calculated with the “Student T test” and the “Wilcoxon test”.
Results
19 patients with acute respiratory failure were recruited: 12 patients were male, 7 were female. The average age was 66 years. Regarding the remote anamnestic report it was documented that 5 were affected by diabetes mellitus, 5 by dyslipidemia, 10 by arterial hypertension, 1 by heart failure, 2 by previous ischemic cardiopathy, 2 by atrial fibrillation, 2 by rheumatological diseases, 1 by chronic renal failure, 3 from psychiatric disorders, 2 from active neoplasia and 4 from thyroid disease. Regarding the proper respiratory history: 9 patients were affected by chronic obstructive bronchopneumopathy, 3 had a previous diagnosis of asthmatic disease, 2 were affected by fibrothorax, 1 had undergone total pneumectomy for previous tuberculosis, and at the end, bronchiectasis were found in 7 patients, 2 of whom were affected by cystic fibrosis.
By analyzing the cause underlying the respiratory failure: 16 patients had pneumonia, 2 patients had pulmonary contusion trauma-related and 1 patient had heart failure. These diagnoses were also supported by labs and imaging findings. All patients in fact performed a chest x-ray in 2 projections and 12 patients also performed a high resolution TC scan.
HFNC were used as first line oxygen-therapy only in 3 cases, in the rest of the patients they have always been used as second line therapy. In particular, at the time of initiating therapy with HFNC, 9 patients underwent oxygen therapy with Ventimask and 7 with Non Invasive Ventilation, including 4 patients treated with CPAP devices and 3 with NPPV ventilators. The mean FiO2 used, before starting the HFNC therapy, was 41.26% (min.21%, max.60%). In the oxygen therapy carried out with HFNC, an initial average FiO2 of 49% (min 26%, max 83%), an average flow of 50 liters/minute (min 40, max 60) was used, with an average temperature of 33°C (min 31°C, max 34°C). The average duration of treatment was 8 days (min 3, max 21).
Once initiating oxygen therapy with HFNC, frequent arterial blood gas analysis were performed after 12, 24, 48 and 72 hours, and one last at treatment withdrawal.
Regarding arterial gas analysis, it was decided to examine only some values considered significant in order to evaluate the severity and the progression of respiratory failure in response to therapy: pH, partial arterial pressure of oxygen (PaO2), PaO2/FiO2 ratio, oxygen saturation of hemoglobin (Sat%), alveolar-arterial oxygen difference (Δ(Aa)O2) and arterial partial pressure of carbon dioxide (PaCO2). For each of these values the minimum value, the maximum value, the mean and the standard deviation of each gas-analysis were examined. At T0 values were: average PaO2 72 mmHg, mean PaO2/FiO2 ratio 189, average Sat% 93%, (Δ(Aa)O2) 179, average pH 7.38 and average PaCO2 49 mmHg. At the same time, the corresponding respiratory rate of the patients was also examined, the mean value was 30 acts per minute.
Statistical analysis of blood gas data showed an overall improvement in hypoxemia after initiation of HFNC treatment. The values that changed with statistically significance were PaO2, Sat%, PaO2/FiO2 ratio, Δ(A-a)O2. When the HFNC treatment was discontinued, the mean PaO2 was 100 mmHg, the mean PaO2/FiO2 ratio was 304, the mean Sat% was 98%, (Δ(A-a)O2) was 93.
No significant variations were observed for what concerns the PaCO2 and the pH that, at the suspension of HFNC therapy, were 42 mmHg and 7.45 respectively.
In particular, the statistical analysis with Wilcoxon test revealed how the values of PaO2 and Sat% were the only ones to differ with statistically significance already after 12 hours from the beginning of HFNC therapy and how this difference persisted at the suspension (see Table 1).
| P value | ||
| PaO2 | Sat % | |
| T1-T2 | 0,0361 | 0,008 |
| T1-T3 | 0,006 | 0,0003 |
| T1-T4 | 0,05 | 0,005 |
| T1-T5 | 0,0353 | 0,001 |
| T1-T6 | 0,00129 | 0,002 |
Table 1. Changes in arterial gas parameters over time: PaO2, Sat%
Regarding the values of PaO2/FiO2rati and Δ(A-a)O2, the statistical analysis instead showed a significant difference compared to initial values, even if in a later phase (see Table 2).
|
P value
|
||
|
PaO2/FiO2 ratio
|
Δ(A-a)O2
|
|
|
T1-T2
|
0,15
|
0,1
|
|
T1-T3
|
0,10
|
0,8
|
|
T1-T4
|
0,17
|
0,9
|
|
T1-T5
|
0,04
|
0,5
|
|
T1-T6
|
<0,001
|
0,004
|
Table 2. Changes in arterial gas parameters over time: paO2/FiO2ratio, Δ(A-a)O2
For what concerns the trend of the parameters of PaCO2 and the pH the statistical analysis showed, respectively, no significant differences for the first and instead a significant difference, but only in a late phase, for the second (see Table 3).
|
P value
|
||
|
PaCO2
|
pH
|
|
|
T1-T2
|
0,37
|
0,442689387
|
|
T1-T3
|
0,7
|
0,130579025
|
|
T1-T4
|
0,6
|
0,054466785
|
|
T1-T5
|
1
|
0,046699777
|
|
T1-T6
|
0,8
|
0,006324938
|
Table 3. Changes in arterial gas parameters over time: PaCO2, pH
Regarding the analysis of PaCO2, a very interesting data was obtained from the application of the Wilcoxon test to the subgroup of patients suffering from hypercapnic respiratory failure. In patients with type II ARF and with initial PaCO2 ≥ 50 mmHg, both the PaCO2 and pH have indeed shown a significant difference already after 12 hours from the start of oxygen therapy with HFNC (see Table 4).
| P value | ||
| Hypercapnia | PaCO2 | pH |
| T1-T2 | 0,0078 | 0,0156 |
| T1-T3 | 0,0078 | 0,0156 |
| T1-T4 | 0,0078 | 0,0156 |
| T1-T5 | 0,0078 | 0,0156 |
| T1-T6 | 0,0078 | 0,0156 |
Table 4. Variations in the subgroup “hypercapnic respiratory failure” of the arterial gas parameters over time: paCO2, pH
A further subgroup analysis was performed for patients with bronchiectasis. The statistical analysis showed on the one hand a statistically significant difference in the PaCO2 values after at least 24 hours, on the other hand a statistically significant difference in pH values already after 12 hours from the start of HFNC (see Table 5).
|
P value
|
||
|
Bronchiectasis
|
PaCO2
|
pH
|
|
T1-T2
|
0,29
|
0,0156
|
|
T1-T3
|
0,0156
|
0,0156
|
|
T1-T4
|
0,0156
|
0,0156
|
|
T1-T5
|
0,0156 | 0,0156 |
|
T1-T6
|
0,0156
|
0,0156
|
Table 5. Variations in the “Bronchiectasis” subgroup of the arterial gas parameters in time: PaCO2, pH
The statistical analysis by Wilcoxon test performed on the respiratory rate parameter showed an important statistical difference already after 12 hours from the beginning of therapy with HFNC over the entire population recruited (see Table 6).
| FR | P value |
| T1-T2 | 0,0006 |
| T1-T3 | 0,0001 |
| T1-T4 | 0,0001 |
| T1-T5 | 0,0001 |
| T1-T6 | 0,0001 |
Table 6. Changes in respiratory rate over time
Discussion
In our prospective observational study, a total of 19 patients with acute respiratory failure were enrolled.
In most cases, the diagnosis through gas analysis resulted in type I ARF (normo/hypocapnic hypoxaemic), and in a minor percentage type II ARF (hypercapnic hypoxaemic). Regarding the treatment of hypoxemia, based on our data, we can state that oxygen therapy with HFNC has proved to be effective. The statistical analysis of the blood gas parameters (6 samples of arterial blood) has in fact shown a statistically significant improvement of PaO2and Sat% just right after 12 hours, then in all successive 4 samples until weaning.
Another important improvement resulted with PaO2/FiO2ratio and Δ(A-a)O2. Respectively PaO2/FiO2ratio showed a statistically significant difference at the fifth blood gas control performed after 72 hours of HFNC therapy; Δ(A-a)O2, showed results at the last blood gas control carried out during the suspension of therapy. In the light of current knowledge we can affirm that the improvements of PaO2and of Sat% are surely linked to the possibility of HFNC to simultaneously deliver high flows and high concentrations of oxygen in the gas mixture inspired by the patient. On the other hand, as regards the change in the PaO2/FiO2ratio and the Δ(Aa)O2, the later improvement could correlate with the slower action of medical therapy, in particular antibiotics, and with the progressive alveolar recruitment linked to PEEP effect produced by the high flow.
Regarding the HFNC treatment of patients with type II ARF, the results were equally interesting. In fact, HFNC were able to determine a statistically significant improvement of all in blood gas parameters related to oxygenation (PaO2, Sat%, PaO2/FiO2ratio, Δ(Aa)O2) and, on the other hand, a marked improvement in PaCO2and pH. In particular, in the subgroup of hypercapnic patients (PaCO2> 50 mmHg), a statistically significant reduction of PaCO2with an increase of pH were already found after 12 hours of treatment, and maintained until the weaning. These results are related to the continuous wash-out of the anatomical dead space with consequent increase in alveolar ventilation. To date, there are not enough studies in the literature to demonstrate how the PEEP effect of HFNC is able to balance the intrinsic PEEP of a patient suffering from a chronic obstructive respiratory deficit. Another important fact that emerged from our analysis was the clear and statistically significant reduction of respiratory rate, even after 12 hours. As is known, this reduction is linearly correlated with the amount of respiratory distress. Most of the patients with enrolled in our study were affected by pneumonia. The therapeutic efficacy of HFNC would seem to be correlated with both the possibility to simultaneously deliver a high flow of oxygen and a high FiO2, but also with the ability of the high flow to create a PEEP effect. It is in fact known that, in the treatment of pneumonia, where conventional oxygen therapy is not able to bring the desired effects, the delivery of a PEEP can play a fundamental role thanks to the alveolar recruitment action. Another winning feature of HFNC is the effect of continuous delivered aerosol through hot and humidified gases, with consequent improvement of ciliary mucus clearance, which led to appropriate mobilization of secretions.
A noteworthy fact is the presence of 32% of patients suffering from pneumonia, but with pre-existing bronchiectasis. Bronchiectasis is a chronic obstructive lung disease characterized by dilatation of bronchi of congenital origin or, more commonly, secondary to repeated pulmonary inflammation (tuberculosis, immunodepression states, pneumonia ab ingestis). In this pathology, characterized by a significant deficit of muco-ciliary clearance, neutrophilic inflammation and the increased production of thick secretions play a fundamental role.
In this subgroup the efficacy of HFNC seems mainly due to the improvement of muco-ciliary clearance, particularly damaged in bronchiectasis, and consequently to the possibility to better mobilizing and eliminating secretions. The relative statistical analysis also showed that a particularly relevant data would seem to be represented by the normalization of the pH and the reduction of the detectable PaCO2 already after only 12 hours of treatment. This data is even more interesting considering that it was often not possible to obtain the same results despite treatment with NPPV.In the sample we examined, it is interesting to note that 37% of the patients, before starting treatment with HFNC, were subjected to NIV: 4 cases of CPAP, 3 cases of NIV. The decision to choose oxygen therapy by HFNC was mostly based on manifest intolerance to both CPAP and NPPV devices.
Moreover, in 3 cases coexisted an important state of psychomotor agitation due to known psychiatric pathology leading to respiratory distress and ARF. It is very common in ED settings, which make NIV hardly feasible and so requiring a constant sedation with high monitorization. In our experience, treatment with HFNC was instead easily managed and well tolerated even by these patients, who could even reject therapy with NIV.
In 1 patient, the decision to not start the NPPV despite evident type II ARF, was instead taken with the aim of avoiding any iatrogenic damage related to the ventilation. This patient had in fact undergone a total pneumectomy developing fibrothorax and bronchiectasis on the residual lung. Even in this case HFNC was a valid alternative to the NPPV. In other 2 cases the HFNC were used for the management of polytraumatic patients who presented severe pulmonary contusion and atelectasis. In particular, in one of them, the abundant blood and mucous secretions had caused, a few days after admission, an important bronchial occlusion needed surgery. It was then decided to treat the patient with HFNC to exploit the PEEP effect in order to help the re-expansion of the lung, and to fluidify and eliminate the abundant secretions. HFNC therapy, combined with effective analgesic therapy, has proved to be particularly useful in these patients because it has moreover allowed them to perform respiratory physiotherapy without interrupting treatment. The results would seem encouraging and reporting for HFNC a rate of orotracheal intubation overlapping to NIV (12-18%).
All of the patients we enrolled mostly showed good compliance with the method and never showed desire to interrupt for manifested intolerance. Moreover, it deserves to be emphasized that HFNC therapy had always allowed patients to feed, drink and talk. And at the end, no complication occurred.
Healthcare professionals who used HFNC reported a high approval, because it is an easy learn method, practice to manage compared to other more invasive methods, such as NIV.
Conclusion
Our study showed that oxygen therapy with HFNC can be a valid therapeutic option in all hypoxemic acute respiratory failure patients. In particular, our sample was represented for the majority (84%) by patients suffering from pneumonia. At the current state of our knowledge the treatment of hypoxemia during pneumonia does not have a unique indication. If for severe pneumonia a patient should be managed in an intensive setting with a prompt invasive management of the airways, for cases of persistent hypoxemia, despite the conventional oxygen therapy, it is allowed the possibility of a cautious and very short NIV trial (1-2 hours).
The most significant risk of treatment with NIV in the management of the hypoxemic patient is the delaying of orotracheal intubation. Today it is a notorious element associated with a higher mortality rate especially in patients not affected by other comorbidities.
In recent years HFNC began to attract with increasing interest the Scientific Community and numerous studies have investigated their effectiveness in the treatment of type I ARF, including that due to pneumonia. Moreover, the FLORALI, the study that has caused the most uproar and that, to date, has marked the most prestigious point in favor of HFNC, has recruited a sample of patients of which 80% affected by pneumonia. The data in our possession would seem to be aligned with these works, confirming the efficacy of oxygen-therapy with HFNC but, in order to not delay orotracheal intubation, the execution of close analysis of blood gasses, especially in the initial phase of therapy, remains a crucial point.
The most significant risk of treatment with NIV in the management of the hypoxemic patient is the delaying of orotracheal intubation. Today it is a notorious element associated with a higher mortality rate especially in patients not affected by other comorbidities.
In recent years HFNC began to attract with increasing interest the Scientific Community and numerous studies have investigated their effectiveness in the treatment of type I ARF, including that due to pneumonia. Moreover, the FLORALI, the study that has caused the most uproar and that, to date, has marked the most prestigious point in favor of HFNC, has recruited a sample of patients of which 80% affected by pneumonia. The data in our possession would seem to be aligned with these works, confirming the efficacy of oxygen-therapy with HFNC but, in order to not delay orotracheal intubation, the execution of close analysis of blood gasses, especially in the initial phase of therapy, remains a crucial point.
In addition, our HFNC analysis was particularly effective in the treatment of patients with type II ARF (PaCO2>50 mmHg), which rapidly achieved a significant reduction in PaCO2 and a normalization of pH.
A surprising result was obtained in the subgroup of patients with bronchiectasis and intercurrent pneumonia. The action of the high flow of heated and humidified oxygen would seem to have an important action in the fluidification and therefore in the mobilization of the secretions, which led to an important reducing of work of breathing and producing a great advantage in those patients affected by primitive muco-ciliary clearance deficit.
Although, the number of patients recruited with hypoxaemia due to thoracic trauma (11%) is extremely limited, but even in this case our experience would seem encouraging.
Another fundamental element is that HFNC therapy is extremely tolerated by patients and therefore represents a valid alternative to NIV in case of poor compliance, even in the weaning from NIV.
In conclusion, we can therefore state that, based on our data, oxygen therapy with HFNC could be on the one hand a valid and effective treatment in patients with hypoxemic acute respiratory failure, and on the other hand a valid alternative to NPPV in the treatment of patients with hypoxemic and hypercapnic respiratory failure, especially if suffering from bronchiectasis. The management of these patients, even if with a not severely low pH, naturally requires a higher level of clinical and instrumental monitoring to avoid the risk of delayed invasive management of airways, where indicated.
For the purpose of its pubblication, the Author declare of not being in condition of conflicting interest, even potential.
Bibliography
- Mardegan V., Priante E., Lolli E., Lago P., Baraldi E. Heated, Humidified High-Flow Nasal Cannulae as a Form of Noninvasive Respiratory Support for Preterm Infants and Children with Acute Respiratory Failure. Am J Perinatol. 2016;33(11):1058-61
- Sinha I.P., McBride A.K., Smith R., Fernandes R.M. CPAP and High-Flow Nasal Cannula Oxygen in Bronchiolitis. Chest 2015;148(3):810–823
- Kelly G.S., Simon H.K., Sturm J.J. High-flow nasal cannula use in children with respiratory distress in the emergency department: predicting the need for subsequent intubation. Pediatr Emerg Care. 2013;29:888—92.
- Wing R., James C., Maranda L.S., Armsby C.C. Use of high-flow nasal cannula supportin the emergency departmentreduces the need for intubation in pediatric acute respiratory insufficiency. Pediatr Emerg Care. 2012;28:1117-23.
- Slaina K.N., Sheina S.L., Rotta A.T. The use of high-flow nasal cannula in the pediatric emergency department. J Pediatr (Rio J). 2017;93(s1):36-45
- Masclans J.R., Roca O. High-flow oxygen therapy in acute respiratory failure. Clin Pulm Med. 2012;19(3):127–30.
- Parke R.L., McGuinness S.P. Pressures delivered by nasal high flow oxygen during all phases of the respiratory cycle. Respir Care. 2013;58(10):1621-4.
- Groves N., Tobin A. High flow nasal oxygen generates positive airway pressure in adult volunteers. Aust Crit Care. 2007;20(4):126-31.
- Parke R., McGuinness S., Eccleston M. Nasal high-flow therapy delivers low level positive airway pressure. Br J Anaesth. 2009;103(6):886-90.
- Parke R.L.., Eccleston M.L., McGuinness S.P. The effects of flow on airway pressure during nasal high-flow oxygen therapy. Respir Care 2011:56(8):1151-1155.
- Parke R.L., Bloch A., McGuinness S.P. Effect of very-high-flow nasal therapy on airway pressure and end-expiratory lung impedance in healthy volunteers. Respir Care. 2015;60(10):1397–403.
- Braunlich J., Beyer D., Mai D., Hammerschmidt S., Seyfarth H.J., Wirtz H. Effects of nasal high flow on ventilation in volunteers, COPD and idiopathic pulmonary fibrosis patients. Respiration 2012 Nov, doi:10.1159/000342027.
- Fricke K., Tatkov S., Domanski U. et al. Nasal high flow reduces hypercapnia by clearance of anatomical dead space in a COPD patient. Respir Med Case Rep 2016;19:115-7.
- Bräunlich J., Köhler M., Wirtz H. Nasal highflow improves ventilation in patients with COPD. Int J Chron Obstruct Pulmon Dis 2016;11:1077-85.
- Ravenscraft S.A., Shapiro R.S., Nahum A., Burke W.C., Adams A.B., Nakos G. et al. Tracheal gas insufflation: catheter effectiveness determined by expiratory flush volume. Am J Respir Crit Care Med 1996:153(6):1817-1824.
- Wood K.E., Flaten A.L., Backes W.J. Inspissated secretions: a life-threatening complication of prolonged noninvasive ventilation. Resp Care 2000: 45: 491-493.
- Williams R., Rankin N., Smith T., Galler D., Seakins P. Relationship between the humidity and temperature of inspired gas and the function of airways mucosa. Crit Care Med 1996:24(11):1920-1929.
- Hasani A., Chapman T.H., McCool D., Smith R.E., Dilworth J.P., Agnew J.E. Domiciliary humidification improves lung mucociliary clearance in patients with bronchiectasis. Chronic Respir Dis 2008:5(2):81-86.
- Richards G.N., Cistuiu P.A., Ungar R.G., Berthon-Jones M., Sullivan C.E. Mouth leak with nasal continuous positive airway pressure increases nasal airway resistance. Am J Respir Crit Care Med 1996:154:182-186.
- Dysart K., Miller T.L., Wolfson M.R., Shaffer T.H. Reseach in high flow therapy: mechanisms of action. Respir Med 2009:103:1400-1405.
- Chanques G., Constantin J.M., Sauter M., Jung B., Sebbane M., Verzilli D., et al. Discomfort associated with underhumidified high-flow oxygen therapy in critically ill patients. Intensive Care Med 2009:35:996-1003.
- Sztrymf B., Messika J., Mayot T., Lenglet H., Dreyfuss D., Ricard J.D. Impact of highflow nasal cannula oxygen therapy on intensive care unit patients with acute respiratory failure: a prospective observational study. J Crit Care 2012:27 324:e9-13.
- Roca O., Hernández G., Díaz-Lobato S., Carratalá J.M., Gutiérrez R.M., MasclansR. Current evidence for the effectiveness of heated and humidified high flow nasal cannula supportive therapy in adult patients with respiratory failure. Critical Care (2016) 20:109
- Messika J., Ben Ahmed K., Gaudry S. et al. Use of high-flow nasal cannula oxygen therapy in subjects with ARDS: a 1-year observational study. Respir Care. 2015;60(2):162–9.
- Lenglet H, Sztrymf B, Leroy C, Brun P, Dreyfuss D, Ricard JD. Humidified high flow nasal oxygen during respiratory failure in the emergency department: feasibility and efficacy. Respir Care 2012:57(11):1873-1878.
- Spoletini G., Alotaibi M., Blasi F., Hill N.S. Heated humidified high-flow nasal oxygen in adults: mechanisms of action and clinical implications. Chest. 2015 Jul;148(1):253-261.
- Fricke K., Tatkov S., Domanski U. et al. Nasal high flow reduces hypercapnia by clearance of anatomical dead space in a COPD patient. Respir Med Case Rep 2016;19:115-7.
- Hasani A., Chapman T.H., McCool D. et al. Domiciliary humidification improves lung mucociliary clearance in patients with bronchiectasis. Chron Respir Dis. 2008;5(2):81–6.
- Rea H., McAuley S., Jayaram L. et al. The clinical utility of long-term humidification therapy in chronic airway disease. Respir Med. 2010;104(4):525–33.
- Miguel-Montanes R., Hajage D., Messika J. et al. Use of high-flow nasal cannula oxygen therapy to prevent desaturation during tracheal intubation of intensive care patients with mild-to-moderate hypoxemia. Crit Care Med. 2015;43(3):574–83.
- Vourc’h M., Asfar P., Volteau C. et al. High-flow nasal cannula oxygen during endotracheal intubation in hypoxemic patients: a randomized controlled clinical trial. Intensive Care Med. 2015;41(9):1538–48.
- Epstein A.S., Hartridge-Lambert S.K., Ramaker J.S. et al. Humidified high-flow nasal oxygen utilization in patients with cancer at Memorial Sloan-Kettering Cancer Center. J Palliat Med. 2011;14(7):835–9.
- Lee H.Y., Rhee C.K., Lee J.W. Feasibility of high-flow nasal cannula oxygen therapy for acute respiratory failure in patients with hematologic malignancies: a retrospective single-center study. J Crit Care. 2015;30(4):773–7.
- Guideline for emergency oxygen use in adult patients. British Thoracic Society Emergency Oxygen Guideline Group.THORAX. 2008.
- Fricke K., Tatkov S., Domanski U., et al. Nasal high flow reduces hypercapnia by clearance of anatomical dead space in a COPD patient. Respir Med Case Rep 2016;19:115-7.
- Mandell L.A., Wunderink R.G., Anzueto A., Bartlett J.G., Douglas Campbell G, Dean N.C., Dowell S.F., File T.M., Musher D.M., Niederman M.S., Torres A., Whitney C.G. Infectious Diseases Society of America/American Thoracic Society Consensus Guidelines on the Management of Community-Acquired Pneumonia in Adults. CID 2007; 44:S27–72
- Rochwerg B., Brochard L., Elliott M.W., Hess D., Hill N.S., Nava S., Navalesi P.- Members Of The Steering Committee, Antonelli M., Brozek J., Conti G., Ferrer M., Guntupalli K., Jaber S., Keenan S., Mancebo J., Mehta S., Raoof S. – Members Of The Task Force. Official ERS/ATS clinical practiceguidelines: noninvasive ventilation foracute respiratory failure. Eur Respir J 2017; 50: 160242
- Ferrer M., Cosentini R., Nava S. The use of non-invasive ventilation during acute respiratory failure due to pneumonia. Eur J Intern Med 2012;23(5):420-8
- Pasteur M.C., Bilton D., Hill A.T. British Thoracic guideline for non-CF Bronchiectasis. British Thoracic Society Non-CF Bronchiectasis Guideline Group. Thorax. 2010;65(7):577
- Halub M.E., Spilman S.K., Gaunt K.A., Lamb K.D., Jackson J.A., Oetting T.W., Sahr S.M. High-flow nasal cannula therapy for patients with blunt thoracic injury: A retrospective study. Can J Respir Ther Vol 52 No 4 Fall 2016



