- Ilaria Ricci Iamino
- Brief Report and Case Report
An unusual case of dizziness: a case report
- 1/2019-Febbraio
- ISSN 2532-1285
- https://doi.org/10.23832/ITJEM.2019.004
Ilaria Ricci Iamino*, Ernesto Gelonesi**
*Unità Operativa di Medicina Interna, Dipartimento Cardio-Toraco-Vascolare, Università di Bologna
**Pronto Soccorso e Medicina d’Urgenza, Ospedale Sant’Orsola-Malpighi Bologna

Abstract
Wallenberg’s syndrome is a neurological disorder usually caused by occlusion of postero-inferior cerebellar artery or vertebral artery. It’s the most common ischemic event of the encefalic trunk and is characterized by misleading symptoms and signs.
When a young boy came to the Emergency Department (ED) with acute dizziness and anisocoria we performed a cranial CT (resulted negative) and we treated him with steroid therapy. We dismissed him at home with the diagnosis of suspected vestibular neuronitis. The day after he showed up again at the ED complaining dysphagia, dysphonia, ataxia and paresthesia of left face and right body.
Angio-CT (CTA) showed a intracranial left vertebral artery dissection and MRI a left bulbar ischemic lesion. He was treated with antiplatelet drugs and after a period of rehabilitation therapy he recovered almost completely.
Keywords
dizziness, vertebral arteries, Wallenberg’s syndrome, vestibulocerebellar symptoms.
Introduction
Case Report
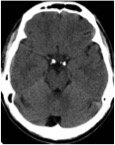
We report the case of a 28-year old man, who came to our observation in the Emergency Department for objective dizziness, vomit, nystagmus to the right and anisocoria (left miosis). He had a negative pathological history and no home therapy. We performed a cranial CT which turned out negative (fig.1). An otholaryngologyst evaluation concluded for suspected vestibular neuronitis; after steroid therapy he felt better, and the patient was then discharged at home.
Figure 1 – axial scan TC: any alteration
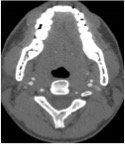
The day after he complained the persistence of dizziness associated with dysphonia, dysphagia, ataxia and paresthesias of left face and right body.Anisocoria was still present (left Horner syndrome). A second cranial TC with CTA showed a left vertebral artery dissection in the intracranial part (fig. 2 and 3).
Figure 2
Figure 3
Discussion
Ischemic events involving posterior cerebral circulation are frequent: they occur, in fact, in about 20% of all ischemic event and are caused by atherosclerosis, embolism and dissection of the large aortic arch, neck and intracranial arteries [2-5]. Arterial dissection is a common cause of posterior circulation stroke which usually involves the proximal extracranial vertebral arteries (ECVAs) just before they enter the foramen transversarium at C5 or C6, or in the very distal part of the artery in the neck before they penetrate the dura mater to enter the cranial cavity [6].
ECVA dissection usually causes vestibulocerebellar symptoms like dizziness, veering to one side, loss of balance and ataxia (when infarct involves the inferior portion of the cerebellum). The involvement of the intracranial part can cause vestibulocerebellar symptoms [7] and other symptoms as hypotonia of the ipsilateral arm, blurred vision or diplopia, nystagmus, ocular torsion and sensory symptoms (pain or unpleasant feelings in the face, loss of pain and temperature sensation in the ipsilateral face and in the controlateral trunk and limbs) [8].
Involvement of the nucleus ambiguus causes hoarseness and dysphagia.
Eventually contralateral hemiparesis is frequent in medial medullary ischemia; paresthesias or dysesthesias in the controlateral limb and trunk are described in ischemia of the medial lemniscus [7-9].
The occlusion of posteroinferior cerebellar artery or vertebral artery defines the “PICA syndrome” also called Wallenberg’s syndrome (first described in 1895). This is the most common ischemic event of the encefalic trunk and it is characterized by a lot of symptoms and signs caused by a stroke of retro-olivar area. Usually it presents with ipsilateral Horner’s syndrome, ataxia, facial loss of pain and temperature sensation and laryngeal muscles paralysis and controlateral hemiparesis and body loss of pain and temperature sensation.
The diagnosis is confirmed by neuroimaging findings (MRI or cranial CT with CTA) [10-12].
The available evidence suggests that treatment with thrombolytic therapy should not be withheld for eligible patients with very early acute ischemic stroke due to extracranial cervical artery dissection. Beyond the hyperacute period, antithrombotic therapy with either anticoagulation or antiplatelet drugs is accepted treatment for ischemic stroke and transient ischemic attack (TIA) caused by extracranial artery dissection, although there is controversy regarding the choice between the two [13]. There is controversy regarding the use of thrombolytics and antithrombotic agents for ischemic symptoms in patients with either intracranial dissection alone or intracranial extension of extracranial dissection because of the presumed increased risk of subarachnoid hemorrhage. Endovascular methods or surgical repair have been used to treat dissection, mainly for patients who have recurrent ischemia despite antithrombotic therapy [14].
The prognosis of cerebral and cervical artery dissection is related primarily to the severity of associated ischemic stroke or subarachnoid hemorrhage. In Wallemberg’s syndrome it’ s usually good with a full recovery in 6 months.
Conclusions
Dizziness is a symptom that can be present in a variety of disease and its presence should lead to look for other neurological symptoms that can help to go on with necessary investigations for diagnosis. In our case, the association of anisocoria, dysphonia, dysphagia, ataxia and paresthesia led us to perform cranial CT with CTA so we reached the final diagnosis of vertebral dissection.
References
1. Brandt T et all Vertigo and Dizziness – Common Complaints. (Vol 2). Springer (2013).
2. Caplan LR, Wityk RJ, Glass TA, et al. New England Medical Center Posterior Circulation registry. Ann. Neurol 2004; 56:389.
3. Savitz SI, Caplan LR. Vertebrobasilar disease. N Engl J Med 2005; 352:2618.
4. Caplan LR. Posterior Circulation Disease: clinical Findings, diagnosis and Management, Black well Science, Boston 1996.
5. Caplan L. Posterior circulation ischemia: then, now and tomorrow. The Thomas Willis Lecture-2000. Stroke 2000; 31:2011.
6. Wityk RJ, Chang HM, Rosengart A et al. Proximal extracranial vertebral artery disease in the New England Medical Center Posterior Cicruclation Registry. Arch Neurol 1998; 55:470.
7. Searls DE, Pazdera L, Korbel E, et al. Symptoms and signs of posterior circulation ischemia in the new England medical center posterior circulation registry. Arch Neurol 2012; 69:346.
8. Matsumoto S, Okuda B, Imai T, Kameyama M. A sensory level on the trunk in lower lateral brainstem lesions. Neurology 1988; 38:1515.
9. Tyler KL, Sandberg E, Baum KF. Medical medullary syndrome and meningovascular syphilis: a case report in an HIV-infected man and a review of the literature. Neurology 1994; 44:2231.
10. Provenzale JM, Sarikaya B. Comparison of the test performance characteristics of MRI, MR angiography and CT angiography in the diagnosis of carotid and vertebral artery dissection: a review of the medical literature. AJR Am J Roentgenol 2009; 193:1167.
11. Vetinsky AT, Schwatz NE, Fischbein NJ, et l. Comparison of multidetector CT angiography and MR imaging of the cervical artery dissection. AJNR Am J Neuroradiol 2008; 29:1753.
12. Provenzale JM. MRI and MRA for evaluation of dissection of craniocerebral arteriea: lessons from the medical literature. Emerg Radiol 2009; 16:185.
13. Chowdhury MM, Sabbagh CN, Jackson D, et al. Antithrombotic treatment for acute extracranial carotid artery dissections: a meta-analysis. Eur J Vasc Endovasc Surg 2015; 50:148.
14. Donas KP, Mayer D, Guber I, et al. Endovascular repair of extracranial carotid artery dissection: current status and level of evidence. J Vasc Interv Radiol 2008; 19:1693.