- Mantuano Stefania
- Brief Report and Case Report
A case of tetanus in the emergency department
- 1/2019-Febbraio
- ISSN 2532-1285
- https://doi.org/10.23832/ITJEM.2019.001
Mantuano Stefania1, Fava Antonio1, Costantino Paolo1, Ianni Angelo2
1. Department of Emergency Medicine and Surgery, Grande Ospedale Metropolitano “Bianchi Melacrino Morelli”, Reggio Calabria;
2. Primary of Department of Emergency Medicine and Surgery, Grande Ospedale Metropolitano “Bianchi Melacrino Morelli”, Reggio Calabria

Abstract
A 68-year-old woman presented to the emergency department affected by tetanus. The patient was promptly treated with antibiotic terapy. Subsequently, the patient was admitted to Intensive Care, despite her general condition were not serious. She was sedated and maxed out on curare; an intubation procedure was made by orotracheal route. Trasferred to the Intensive Care Unit,she was sedated by Fentanest and Diazepam in continuous infusion, began antibiotic intravenoustherapy with Ampicillin/Sulbactam 6 g x 3 times a day for 10 days and she continued the therapy with Metronidazole 500mg 4 times a day. After 18 days of hospitalization in the Intensive Care Unit, the patient was subsequently moved to a rehabilitation unit for further treatment. Studies have shown that inadequate vaccination and no-treatment of wounds remain the most important factors associated with tetanus. According to data from the international literature, older people are more likely to suffer from tetanus and mortality increases considerably over 65 years.
Keywords
Case Report
- a certain degree of cervical stiffness
- difficulty in the motility of the upper left limb.
- her abdomen was widely painful and not very treatable.
- her blood pressure was 155/80mmHg
- her body temperature was 37.8 degrees C.
Figure 1
- intramuscular therapy with specified Human Antitetanic Immunoglobulins (500 U.I. im)·
- 4 gr Ampicillin + 2 gr of Sulbalctam (3 times a day) ·
- Metronidazole 500 mg 1 fl (4 times a day)
Discussion
Tetanus disease is an acute infectious disease caused by Clostridium tetani(Gram-positive, anaerobic, sporogenous bacillus) (photo 2) characterized by localized or generalized muscular hypertonia with paroxysmal exacerbations (spasms or tetanic accesses). The pathogenic action of Clostridium tetaniis carried out through the production of a powerful neurotoxin exotoxin (tetanospasmin) which is fixed to gangliosides, determining, in this way, the suppression of synaptic inhibition. Clostridium tetaniand its spores penetrate the body through continuous solution of the skin or mucous membranes contaminated with debris or ground.
Figure 2
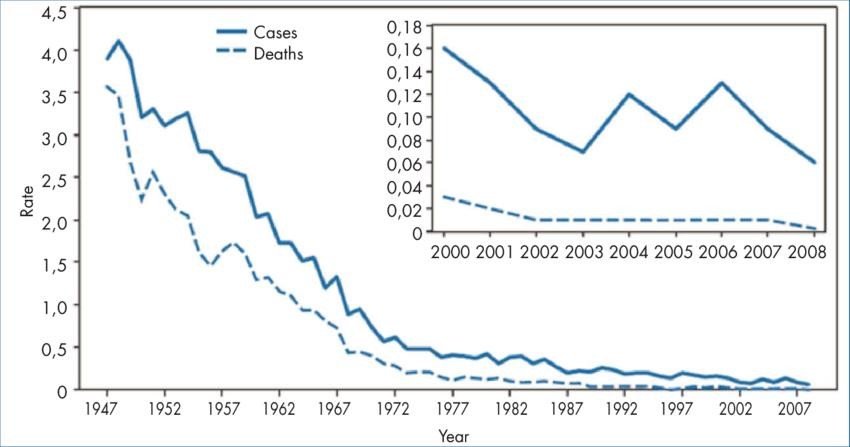
Table 1 – Annual rate* of tetanus cases and tetanus deaths – National Notifiable Diseases Surveillance System, United States, 1947–2008
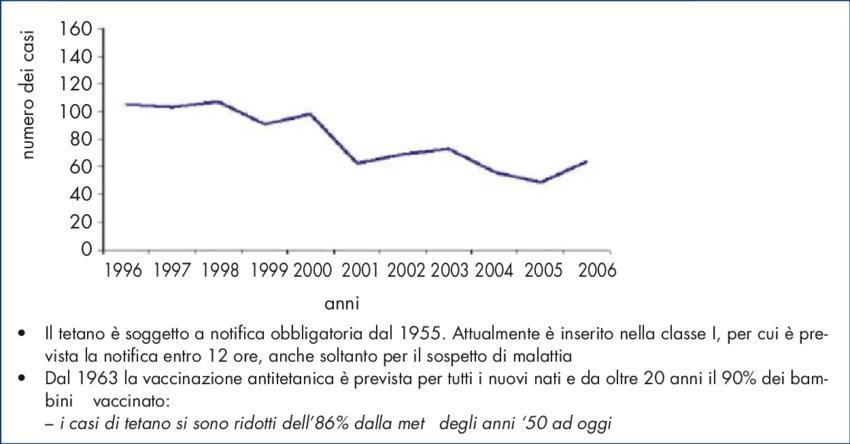
In Italy, 56 cases of tetanus were reported in 2004, 49 cases in 2005, 64 cases in 2006, 62 cases in 2009, and mostly they were elderly people, as in the United States (4).
Clinical Picture
- culture examination of the wound tissue frustules
- biological test.
- Hospitalization in the Intensive Care Unit
- Support vital functions (BLS) if necessary: control and maintenance of airway patency, ventilation and circulation.
- Assess the state of consciousness (pupillary response, osteotendine reflexes, verbal and/or motor response) using the “Glasgow Coma Score”
- Passive immunization: human antitetanic immunoglobulins: 500 U.I. im
- Antibiotic therapy.
- Treatment of paroxysmal access involves the administration of benzodiazepines which, due to their GABA-ergic action, antagonize the action of tetanus toxin:
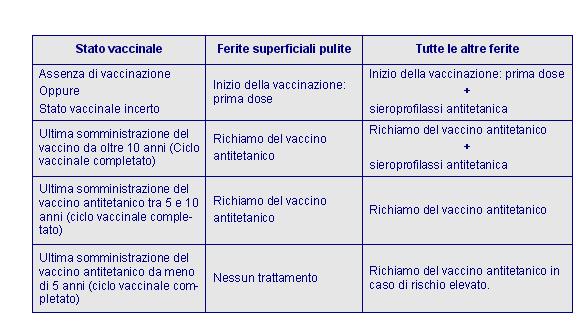
Table 3 – Italian Ministry of Health, circular n° 16 of 11.11.1996
Conclusions
Bibliografy
-
Wright PG. The neurotoxins of Clostridium botulinum and Clostridium tetani. Pharmacol Rev 1955; 7: 413-65.
-
Nowalk MP, Zimmerman RK, Cleary SM, Bruehlman RD. Missed opportunities to vaccinate older adults in primary care. J Am Board Fam Pract2005; 18: 20-27
-
Abbate R, Di Giuseppe G, Marinelli P, Angelillo IF, Collaborative Working Group. Appropriate tetanus prophylaxis practices in patients attending Emergency Departments in Italy. Vaccine2008 4; 26 (29-30): 3634-9
-
[Filia A, Bella A, von Hunolstein C, Pinto A, et al. Tetanus in Italy 2001-2010: a continuing threat in older adults. Vaccine. 2014;32(6):639-44]
-
Monti, M. Filippucci, F. Borgognoni, G.M. Vincentelli. Infezione da tetano: un case report in Pronto Soccorso. Una diagnosi semplice ma spesso sottovalutata nei Pronto Soccorso italiani. ITJEM –Gen. 2013


