- Flora Ilaria Laurino
- Original Article
Hypertensive urgencies and pseudo-urgencies in the Emergency Dept: a proposal of new health-care model in chronic diseases
- 2/2018-Luglio
- ISSN 2532-1285
- https://doi.org/10.23832/ITJEM.2018.021
Flora Ilaria Laurino MD, Nertil Kola MD, Raffaele Izzo MD, Maria Assunta Elena Rao MD, Francesco Rozza MD, Nicola De Luca MD, Marco Mirra MD
Department of Advanced Biomedical Sciences, Federico II University, Naples, Italy

Abstract
Blood pressure (BP) values are extremely variable clinical parameters not only in patients with arterial hypertension but also in the general population. Behind the diagnosis of arterial hypertension there are three different clinical conditions: urgency, emergency and pseudohypertension.
The hypertensive urgency is characterized by high values of PA (> 180/120 mmHg), associated or not with the presence of clinical symptoms, in the absence of acute target organ damage. The presence of organ damage, on the other hand, characterizes the hypertensive emergency. Pseudohypertension is defined as confounder elevated recordings of PA due to high vascular stiffness, white coat hypertension, other comorbidities, anxiety and concerning status.
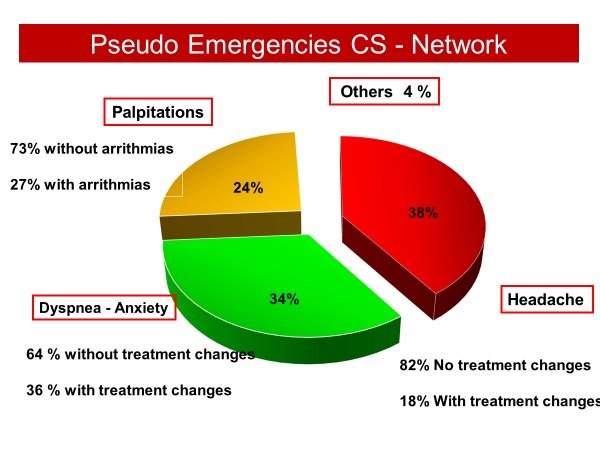
We evaluated, at the Hypertension Center of the University of Naples Federico II, within the “Campania Salute” register, more than 10,000 patients with different cardiovascular risk, of which 984 (9.2%) required an emergency visit for several clinical pictures such as chest pain and / or dyspnoea, palpitations, vertigo and / or lipotymia and headache associated with elevated pressure values >180/110 mmHg. These patients were predominantly female (56%) and with an average age of 64 ± 11 years. The most frequent reasons for requesting a medical examination were hypertension associated with headache (38%), dyspnea / anxiety (34%) and palpitations (24%). Among all symptomatic patients who received headache only in 18% a therapy modification was performed after the visit, while in patients with dyspnoea and / or anxiety the therapy was changed in 36% of cases. Finally, only in 27% of symptomatic patients for palpitations has been found an arrhythmia to the ECG, making necessary therapeutic drug modifications.
From the analysis of this retrospective study it is suggested an implementation of new health-care models for the management of patients with chronic diseases in order to promote compliance with therapy, prevent co-morbidities and mortality, reducing unnecessary hospitalizations.
Keywords
Campania Salute Project, Outpatient Clinic, Arterial hypertension, Pseudohypertension.
Introduction
Methods
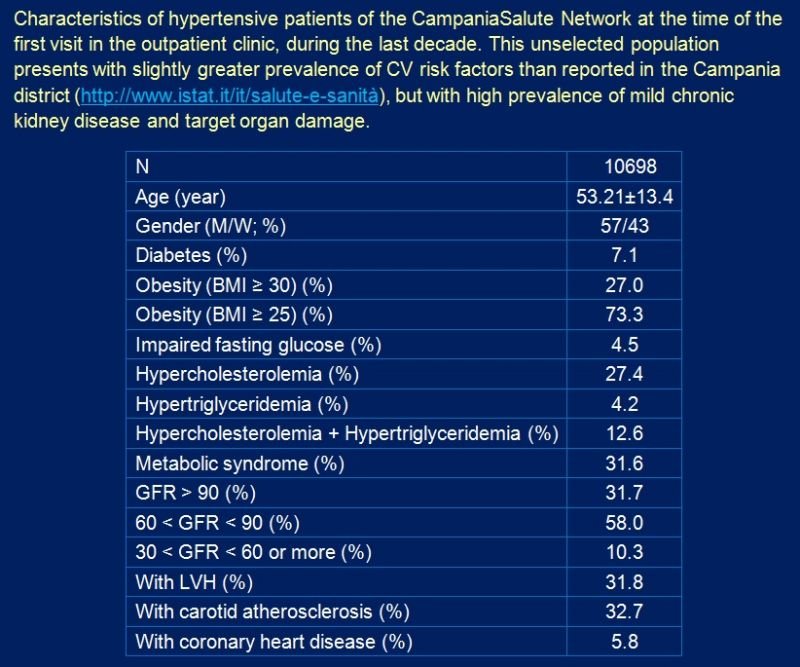
Table 1. Campania Salute Registry study population
Results
Fig.1. Campania Salute Network – Follow-up Pseudo-Emergencies
Discussion
The clinical evaluation in hypertensive urgency begins with the treatment of anxiety and underlying pain, reassuring the patient and possibly administering in anxiolytic or an analgesic, but looking for any symptoms or signs of alarm such as severe headaches, changes in the state of consciousness, convulsions, signs focal neurological disorders, changes in the visus, chest or abdominal pain, dyspnoea, pulmonary / peripheral edema, oliguria.
Conclusions
It is important to implement a new organizational model for an optimal collaboration between the local doctor and the specialist reference center to instruct patients with chronic degenerative diseases to increase compliance with the therapy and manage any critical issues that do not often require access to the Emergency Department.
The severity of AH is not related to the BP measured values, but rather depends on the possible involvement of one or more target organs. It is important to distinguish the urgent causes that endanger the patient life due to the involvement of the target organ and that require an immediate clinical evaluation and the non-urgent causes, without injuries of the target organs, which can be evaluated and treated in the course of the hours following the hypertensive crisis.
It is always necessary to look for factors that affect pressure values to obtain the most standardized, accurate, accurate and reliable BP estimation and to instruct the patient for home measurements. The objective of the management of hypertension through an organized path in the Reference Center is to reduce comorbidity and mortality but also the number of patients who for this reason go to the always overcrowded emergency room.
References
- Mancia G, De Backer G, Dominiczak A et al. 2007 Guidelines for the management of arterial hypertension: the Task Force for the Management of Arterial Hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC) J Hypertens. 2007;25:1105–1187.
- Whelton PK, Carey RM, Aronow WS et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults: Executive Summary. J Am Coll Cardiol. 2017: S0735-1097(17)41518-X.
- Mehlum MH, Liestøl K, Kjeldsen SE et al. Blood pressure variability and risk of cardiovascular events and death in patients with hypertension and different baseline risks. Eur Heart J. 2018 [Epub ahead of print].
- Campos CL, Herring CT, Ali AN et al. Pharmacologic Treatment of Hypertensive Urgency in the Outpatient Setting: A Systematic Review. J Gen Intern Med. 2018 [Epub ahead of print].
- Kleman M, Dhanyamraju S, DiFilippo W. Prevalence and characteristics of pseudohypertension in patients with “resistant hypertension”. J Am Soc Hypertens. 2013;7(6):467-70.
- Boubouchairopoulou N, Karpettas N, Athanasakis K et al. Cost estimation of hypertension management based on home blood pressure monitoring alone or combined office and ambulatory blood pressure measurements. J Am Soc Hypertens. 2014;8(10):732-8.
- Moran AE, Odden MC, Thanataveerat A et al. Cost-effectiveness of hypertension therapy according to 2014 guidelines.N Engl J Med. 2015;372(5):447-55.
- Izzo R, Stabile E, Esposito G et al. Prevalence and characteristics of true and apparent treatment resistant hypertension in the Campania Salute Network.Int J Cardiol. 2015;184:417-9.
- Mancia G, Fagard R, Narkiewicz K et al. 2013 Practice guidelines for the management of arterial hypertension of the European Society of Hypertension (ESH) and the European Society of Cardiology (ESC): ESH/ESC Task Force for the Management of Arterial Hypertension.J Hypertens. 2013;31(10):1925-38.
- Maraj S, Figueredo VM, Lynn Morris D. Cocaine and the heart. Clin Cardiol. 2010 May;33(5):264-9. doi: 10.1002/clc.20746. Review.
- Grassi et al, J Clin Hypertens 2008;10:662–667
- Tsapatsaris NP, Napolitana GT, Rothchild J. Osler’s maneuver in an outpatient clinic setting.Arch Intern Med. 1991;151(11):2209-11.