- Alfonso Sforza
- Brief Report and Case Report
Detection of left atrial compression by focused cardiac ultrasonography in a patient with worsening dyspnea
- 3/2017-Ottobre
- ISSN 2532-1285
- https://doi.org/10.23832/ITJEM.2017.024

Abstract
Keywords
Thrombotic Thrombocytopenic Purpura, microangiopathic haemolytic anaemia, thrombotic events, multiorgan damage, plasmapheresis.
Introduction
Thrombotic Thrombocytopenic Purpura (TTP) is an acute syndrome characterized by the presence of microangiopathic haemolytic anaemia and thrombocytopenia.
The first case of TTP was described by Moschowitz in 1924 [1]. Recently, between 1982 and 2001, several authors [2-5] identified in the deficiency of the metalloproteinase ADAMTS13 the primary pathogenic cause. TTP is a rare disease [6-8]. it occurs between 30 and 50 years of age, more frequently in the female sex. In the absence of treatment, mortality exceeds 90%, while it is reduced to 10-20% after adequate plasma plasmapheresis or infusion therapy. However, half the deaths are attributable to complications associated with plasmapheresis and hospitalization (sepsis, haemorrhages, thrombosis, etc.) [9]
Case Presentation
A 62-year-old man with history of gastric cancer presented to our Emergency Department (ED) with progressive dyspnea and reduced exercise tolerance during last weeks. At admission blood pressure was 110/70 mmHg, heart rate 70 beats/minute regular, oxygen saturation was 98% (FiO2 21%) with mild tachypnea (22 Breaths per minutes) and he was afebrile. Chest examination revealed decreased vesicular murmur in the base of left lung. Cardiovascular examination revealed a normal cardiac rhythm, no murmurs, normal peripheral pulses and no edema. Arterial blood gas analysis on room air revealed respiratory alkalosis with mild hypoxemia. The ECG showed sinus rhythm with normal AV conduction, normal axis and QT interval.
Results of blood tests showed a normal white blood cell count (6.660 cells per mm3), with renal and liver function test and serum electrolytes within the reference limits.
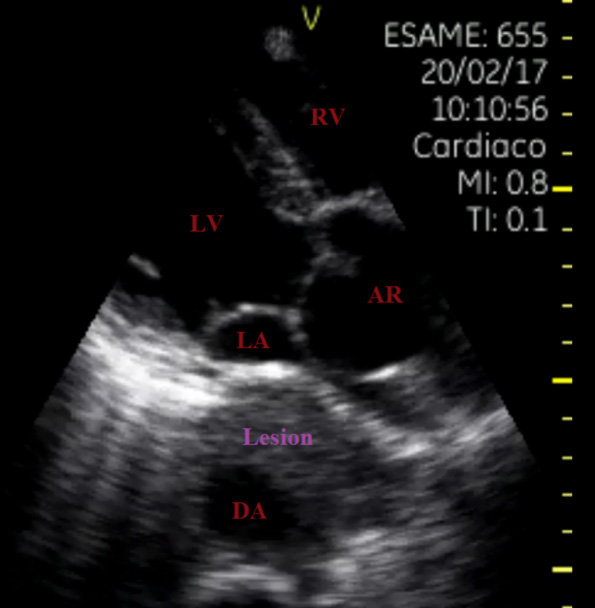
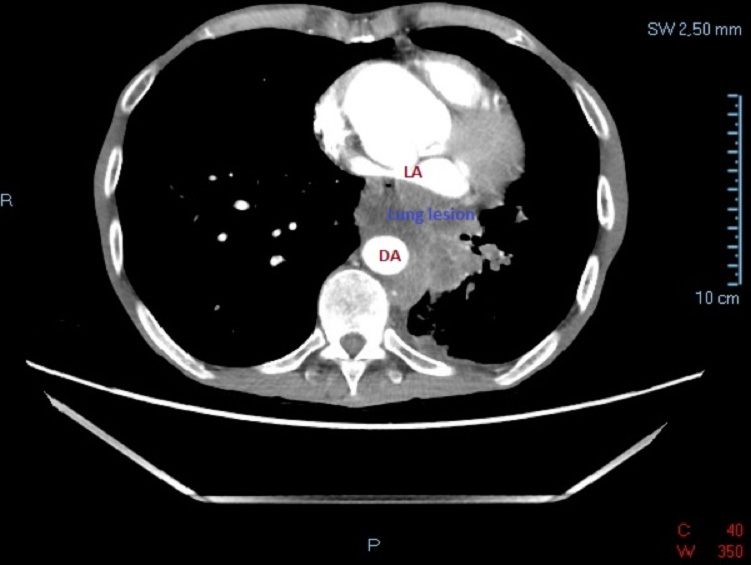
Focused cardiac ultrasonography (FoCUS) showed normal left ventricular (LV) size and function with annuloaortic ectasia and compression of left atrium (LA) due to a large mass englobing the descending aorta (DA) (Figure 1). Lung ultrasonography (LUS) revealed bilateral A-line pattern.
Discussion
Financial/nonfinancial disclosures
References
- Walpot J, A. B. (J Am Soc Echocardiogr. 2007 Oct;20(10):1220.e4-6. Epub 2007 Jun 20). Left atrial compression by dissecting aneurysm of the ascending aorta.
- van Rooijen JM, v. d. (Eur J Echocardiogr. 2008 Sep;9(5):661-4.). Left atrial impression: a sign of extra-cardiac pathology.
- Bouzas-Mosquera A, B.-C. E.-V.-B. (Rev Esp Cardiol. 2008 Jan;61(1):98-9). Left atrial obliteration due to an aortic aneurysm secondary to chronic aortic dissection.
- Mahajan K, A. S. (BMJ Case Rep. 2016 Jan 28;2016. pii: bcr2015214213). Left atrial impression by a dilated oesophagus in a patient with limited cutaneous systemic sclerosis.
- Sforza A, M. C. (Cardiovasc Ultrasound. 2017 Jun 19;15(1):16). Diagnostic performance of multi-organ ultrasound with pocket-sized device in the management of acute dyspnea.