- Livio De Angelis
- Brief Report and Case Report
“Welcome baby girl” in the ambulance: an experience of the Operative Center of Rome. Dispatch and management of a rapid labor
- 2/2017-Giugno
- ISSN 2532-1285
- https://doi.org/10.23832/ITJEM.2017.002
Livio De Angelis, Lorella Calafato, Lucrezia Dell’Aquila, Nadia Latrofa, Stefania Onorini, Carlo Gaetano Claudio Piccolo, Cinzia Vanzo
Azienda Regionale per l’Emergenza Sanitaria 118 Lazio UOC SUES Roma Città Metropolitana
Abstract
Recently there has been an increased incidence of childbirth in pre-hospital setting due to a socio-cultural change in our society. Obstetric emergencies represent a real problem for the Emergency sanitary service, both for a little adequate specific training of the first aid team, both because of the particular emotional involvement that these kind of emergencies. To be able to respond to any request for help, the local emergency service Azienda Regionale per l’Emergenza Sanitaria (ARES) 118 in Lazio, Italy, provides internal courses aimed to acquire specific skills that allow staff to provide appropriate assistance to the new mother and the newborn.
Introduction
During the last years, it has been observed an increased incidence of childbirth in the pre-hospital setting as a consequence of social and cultural changes in our society, and of the increased number of immigrant and indigent women, who have an increased risk of rapid labor. This is characterized by rapid onset of labor, valid contractions, rapid cervical dilation and accelerated progression of the presenting part in the birth canal. Some characteristic labor’s signs cannot be present; often the membranes are intact, and sometimes the mother does not perceive uterine contractions as painful so that she is surprised and not prepared to the fetus’ expulsion(1).
In this context the ARES 118 has to deal with women in labor more frequently: in most cases the intervention ends with the transportation of the patient to the hospital.
But sometimes the birth of the newborn occurs in circumstances and unusual places: in the car, in the elevator, on the street or in the ambulance(2) and in 2016, out of a total of 312.648 relief managed by the Main Emergency Control Office (CO) City of Rome, about 2100 concerned issues related to pregnant women: in 47 cases the information obtained by telephone interview suggested the high probability of imminent childbirth and there have been 16 cases of childbirth at home(3).
Specific courses on obstetric emergencies represent a very important training for the operator, in order to provide specific practical skills and also to prepare the staff to the particular emotional involvement that could occur in this context of care.
Case Report
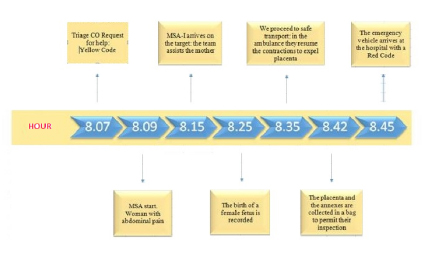
Phase 1: dispatch CO
8.07 a.m.: The telephonic triage of the CO receives a request for help and investigates signs and symptoms according to existing protocols in the CO of Rome[4]; in case of communication difficulties the operator uses a particular scheme of simultaneous multilingual translation. The calling is made by a woman of foreign nationality, which calls for unspecific abdominal pains; the operator give to her a yellow code and sends an advanced equipped emergency vehicle with nurses on board (MSA-I).
Phase 2 – Prehospital care
8.09 a.m.: the MSA-I starts from the control office; Information received: woman with abdominal pain, yellow code.
8.15 a.m.: the MSA-I arrives on site. In the house there is a 31 years old woman of foreign nationality, sitting on the ground and slightly uncooperative, referring abdominal pain from about three hours. She does not report pregnancy and vital signs (VS) are normal.
The nurse reassures the woman[5], and after making her lie, she observes a protruding abdomen, as for full-term pregnancy. After obtaining the consent to the visit, she detects the presence of contractile activity, valid and intense; the observation of the external genitalia shows a relaxed perineum and the appearance of the fetal head by vulvar fissure. The correct evaluation of these elements leads the nurse to establish the imminence of childbirth (1) and after contacting the CO doctor for sending a standard emergency vehicle, the team prepares to attend the laboring woman placing her legs bent, wide apart, with the hands under the knees and placing a tarp over a clean towel under the pelvis. After disinfecting the perineum and vulva, the woman is asked to practice prolonged expulsive efforts (after a deep breath with closed glottis), synchronous with the uterine contractions. The operator lifts her head and places his chin on his chest in order to facilitate the contraction of the abdomen. During the head’s disengagement, the nurse places a gauze in the perineum to allow a better grip on the tissue and to protect the area against spontaneous lacerations. After the fetu’s head has been disengaged, the nurse cleanses the eyes, rims and mouth of the infant, and the woman is invited to relax. After the spontaneous rotation of the fetal head to the maternal thigh (return movement), the nurse made the check of the umbilical cord and she observes a bend around the baby’s neck: she loosens the cord and releases it by passing it around the head. Then the woman is invited to take voluntary abdominal contractions: the trunk of the fetus, the pelvis and the lower limbs are expelled quickly and without difficulty.
8.25 a.m.: the birth of a female fetus is recorded. The child is placed on the same plane of the mother in order to avoid a decrease of the circulating blood volume in the newborn[6]. The standard emergency vehicle arrives so that the physician can assist and support the fetus in the transition to the extra-uterine life. After the baby is dried and stimulated, he begins spontaneously to breath and he starts to cry; the evaluation of a good muscle tone and a heart rate of 160 bpm, allows the assignment of an Apgar score between 7 and 9. After a few minutes after the birth, the doctor clamps the umbilical cord placing a first umbilical clamp to 15-20 cm from the abdomen of the infant and a second at about 5-7 cm from the first in the fetal direction; to prevent the risk of hypothermia, the infant is placed directly in contact with the skin of the mother and then both are covered[7]. The doctor checks the uterus position placing a hand below the navel up to the detection of the fundus[8]. He evaluates the VS (that are normal), he does not observes excessive bleeding from external genitalia, but there is a small bleeding laceration that he stops with direct compression to facilitate hemostasis.
8.35 a.m.: Considering that maternal and neonatal clinical parameters are good, their safety transport to the hospital is planned[9]. The resumption of uterine contractions during transport indicates placental detachment, showed by the cord’s lengthening. With some difficulty due to the restricted environment within the sanitary cell, the team is preparing to the annexes’ expulsion: the doctor applies a downward pressure on the uterus to facilitate the placenta emission.
8.42 a.m.: The placenta and the annexes are collected in a bag to permit their inspection by the hospital specialist staff. It is estimated a discrete physiological loss of blood less than 500 cc.
8.45 a.m.: the emergency vehicle arrives at the hospital with a Red Code and the mother and daughter are entrusted to hospital care.
Discussion
This case report describes a precipitous delivery taking place at home, by a young foreign woman who does not speak the Italian language and entering into the system 118 unclearly. An event quite naturally as the childbirth took place without much difficulty. It was handled appropriately, both by the nursing leadership team, than by doctor. The correct identification of the obstetric emergency and of the critical level, has resulted in the choice of the Stay and Play strategy. The subsequent care interventions allowed to offer an appropriate assistance to the woman in labor and to the child.
Take home message
- The special conditions at birth, can need the “assisted transition” to support the transition to extrauterine life, up to the resuscitation maneuvers (7);
- the body temperature of the infant at birth is strongly associated with infant mortality / morbidity; to avoid the risk of hypothermia the bandage of the body and of the head can be made with plastic film and thermal pads (7);
- the absence of uterine globe can result in excessive bleeding, greater than 500cc, aggravating the clinical condition of the woman in labor. In this case, in addition to uterine massage, it is appropriate to administer oxytocin and infuse liquids, interventions aimed to stabilize the patient hemodynamically(10).
Bibliografia
- Pescetto G, De Cecco L, Pecorari D, Ragni N. Ginecologia e Ostetricia. 2009;cap.35:205/221
- De Luca G, Di Mola F, Ravasi S, Ronzani C, Sangalli F. Il parto imminente: dispatch e gestione extra-ospedaliera; N & A mensile italiano del soccorso, vol 187 maggio 2008
- ARES 118 UOC SUES Roma Città Metropolitana. Relazione sulle Prestazioni e sui Risultati anno 2016
- Progetto I Mattoni del Servizio Sanitario Nazionale: Pronto Soccorso e Sistema 118.Milestone 1.3 – Definizione del sistema di valutazione dei pazienti (triage PS e 118)
- Bertolini R, Bombardi S, Manfredini M. Assistenza Infermieristica e Ostetrica Transculturale. Siliberto; 3 agosto 2010.
- Babies born before arrival at hospital. Br. J Obst & Gynaec. Jan. 1991;98(1):5764
- Wyllie J, Bruinenberg J, Roehr C C et altri. Linee guida European Resuscitation Council per la Rianimazione 2015. Sezione 7:253
- Nappi C. Ostetricia & Ginecologia. Ed. Idelson-Gnocchi. Ristampa 2005, Napoli.
- The Society of Obstetricians and Gynaecologists of Canada. Guidelines form Physicians and Nurses in Maternal/Fetal transport. SOGC Guideline; October 2005 (replaces).
- Truhlaˇr A, Deakin C D, Soar J et altri. Linee guida European Resuscitation Council per la Rianimazione 2015. Sezione 4:190