- Zio Isabella, Groff Paolo
- Area giovani
The use of noninvasive mechanical ventilation in blunt chest trauma. Experience in an elderly patient
- 2 - Maggio 2013
- ISSN 2532-1285
Abstract
Traumatic events in elderly population are steadily increasing for the sharp increase in the proportion of this population on the whole, and for the very active lifestyle that it is now adopting, and represent a significant clinical and prognostic challenge for operators in the ER.
Falls are the most common cause of trauma in the elderly, with particular regard to blunt chest trauma with rib fractures, the prognosis of which linearly worsens with the number of fractures involved. Chest trauma in the elderly triggers a series of consequential pathophysiological mechanisms that determine the early onset of dramatic respiratory failure. The use of non invasive ventilation (NIV) in this condition is still poorly investigated.
We describe a case of blunt chest trauma with “flail ribs” in an elderly patient successfully treated with NIV, occurred in our Emergency Department.
{pub}
Full-text articles are available to registered users for FREE. Please login to access the full article, or register.
{/pub}
{groups:registered,administrator,super users}
Background
Evidence is growing on the use of NIV in patients with chest trauma: Some studies confirm the advantage of this technique compared both to simple oxygen therapy and conventional ventilation, with significant improvements in blood gases, heart rate and respiratory rate, already at 1 h after beginning, and a lower in- hospital mortality and rate of nosocomial infection (1, 2, 3, 4).
Further more, reported complications related to NIV are milder than in intubated patients, mainly nasal ulcers and gastric distension. For these reasons, NIV has been proposed as first choice treatment in the absence of contraindications. In the lack of clinical response or patient’s compliance intubation is to be indicated (1). Our experience confirms the efficacy and good tolerability of NIV in blunt chest trauma also in a variety of patients as complex as that of the elderly, characterized by significant comorbidities.
Case Presentation
An 87 years old woman presents to the ER accompanied by her son, reporting a commotive head injury and closed chest trauma as a consequence of an accidental fall at home getting out of bed. She mostly complains of chest pain, exacerbated by breaths and trunk movements.
The clinical history of the patient shows HCV liver disease, cognitive impairment, COPD in OTLT.
Vitals at presentation are: BP 140/90; HR 77; RR 25; O2-saturation 93% breathing with a 24% Venturi mask; NRS (Numeral Rating Scale) 6; ISS (Injury Severity Score) 25; GCS 13/15.
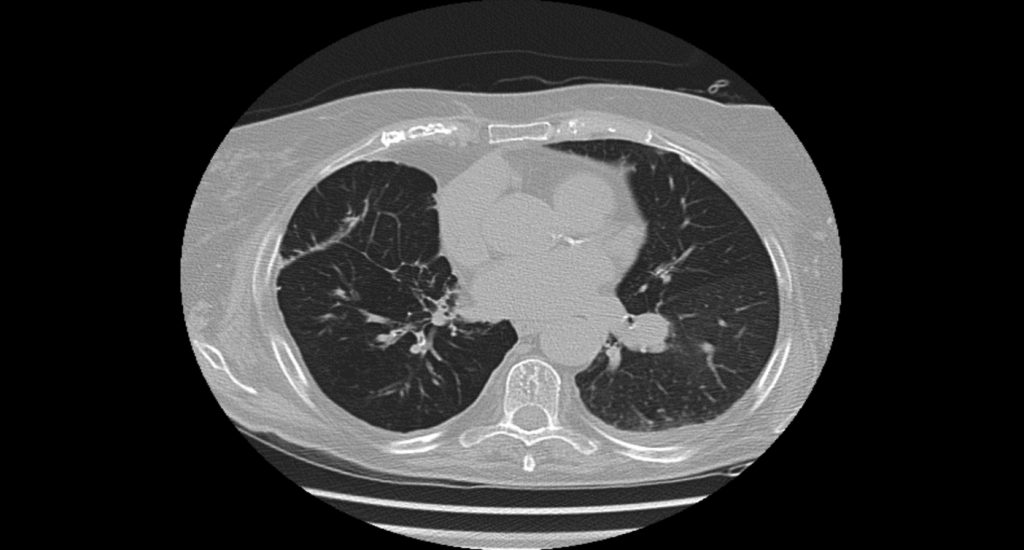
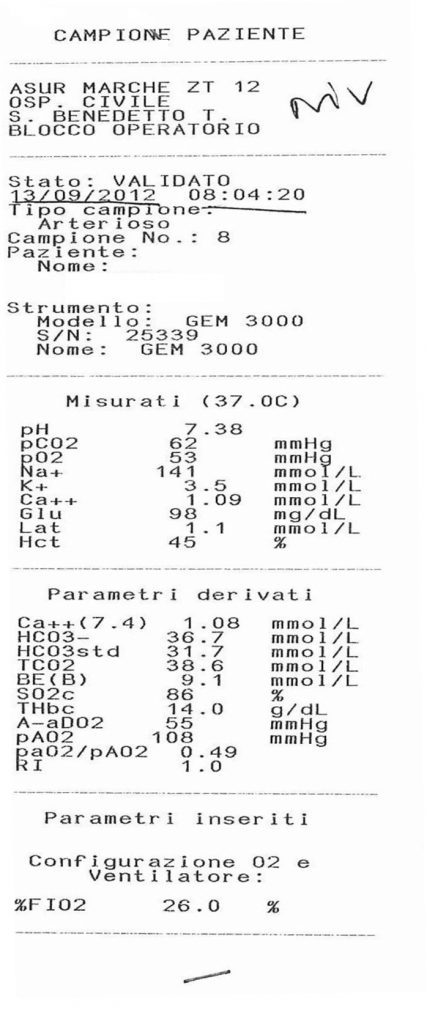
The patient undergoes primary and secondary surveys according to ATLS guidelines. EKG, laboratory tests, BGA are performed (figure 1); peripheral venous catheter, urinary catheter and cervical collar are positioned; O2 therapy is administered.
Investigations
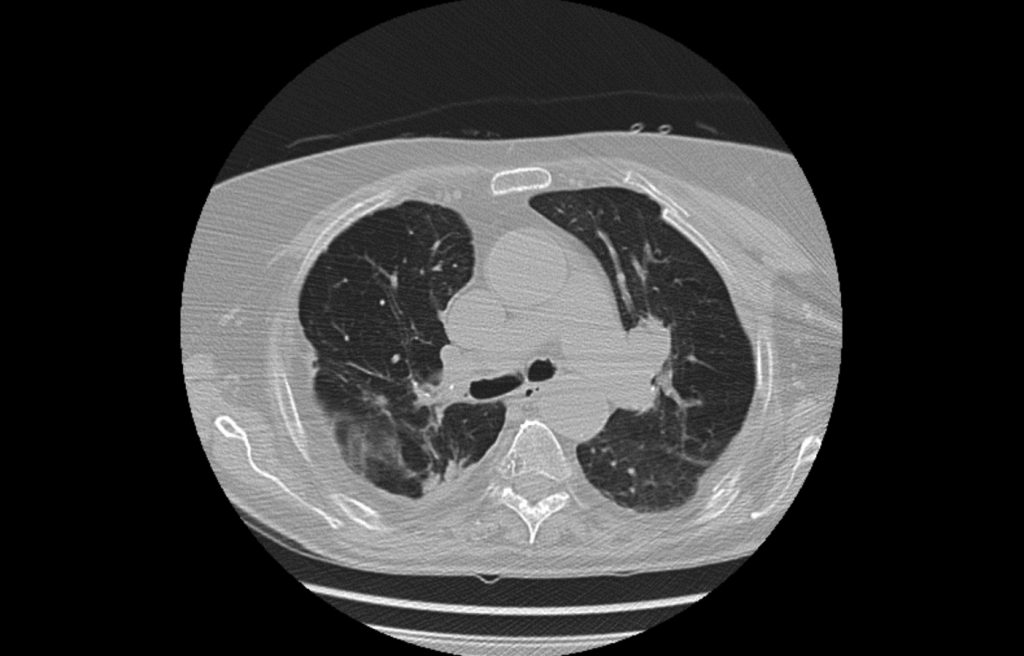
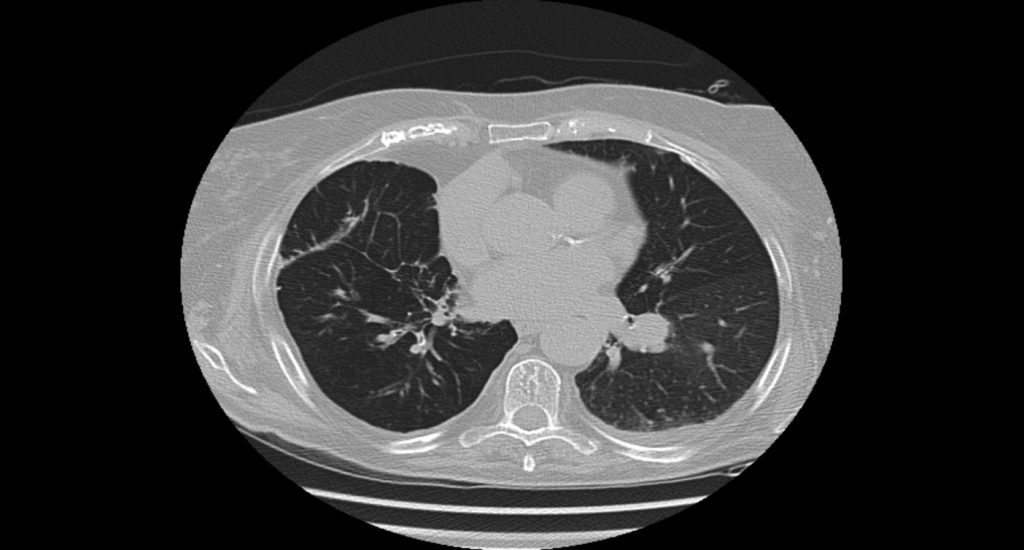
The chest CT scan shows multiple rib fractures, with bifocal character, from the III to the V, in the left hemithorax. No traumatic lesions of the sternum. Moderate pleural effusion in the left hemithorax. No signs of PNX on a framework of COPD (figure 2 and 3).
Figure 2.
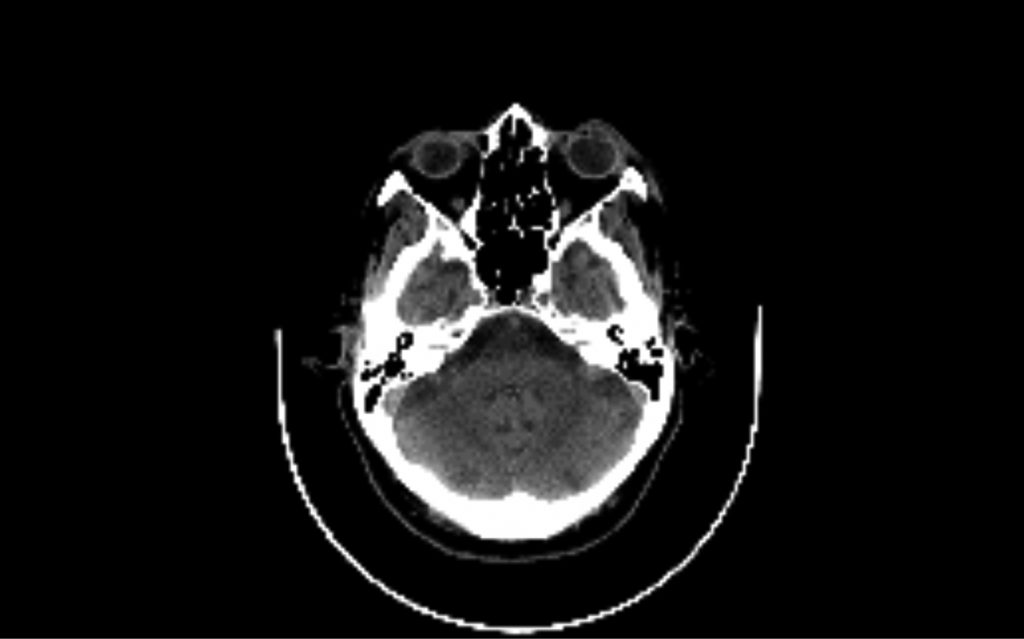
The brain CT scan shows a millimeter layer of subdural left hyperdensity on a framework of marked cerebral leukoencephalopathy (figure 4).
Figure 4
Differential diagnosis
One difficulty in this patient is to establish the priorities for action: head injury or chest trauma. The patient presents with head injury complicated by a minimal hemorrhagic lesion and acute on chronic respiratory failure due to flail chest. GCS is 13 at presentation and the patient slightly confused (probably related to dementia), but BGA and respiratory signs tell us that this patient is not breathing well. Thoracic lesions lead to life-threatening pathophysiological changes such as hypoxia, hypercapnia and acidosis. It is therefore essential to stop the cascade of events to prevent the evolution to SIRS-MOF giving priority to the stabilization of respiratory function.
Treatment
The therapeutic intervention was aimed at ensuring adequate oxygenation and ventilation through the application of NIV, and reducing pain to improve chest compliance and tolerance to treatment through the administration of opioids, in order to prevent possible complications such as infections and atelectasis (5) .
Outcome and follow-up
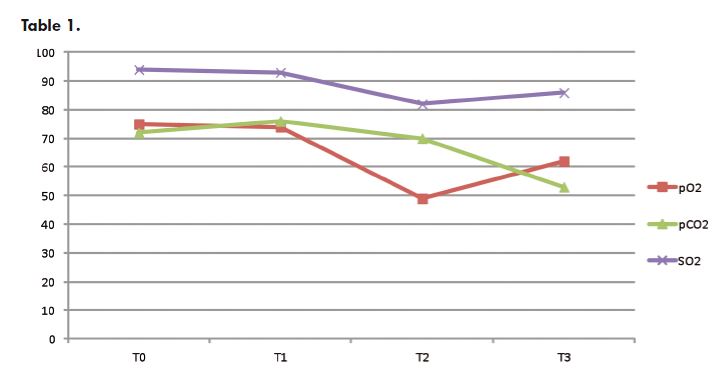
Our patient is therefore subjected to NIV with a full-face mask, 24 cm H2O pressure support, 5 cm H2O PEEP, 26% inspired oxygen fraction, with short breaks for aerosol therapy and nutrition, for 5 days. In the PSV mode, the patient triggers the ventilator to deliver a variable flow of gas until the airway pressure reaches the selected limit. The setting is adjusted to provide the lowest pressure necessary to get a better gas exchange and patient comfort. The results are checked by continuous monitoring of pulse oximetry and expired tidal volumes. BGA is assessed one our after starting ventilation and subsequently every four hours. A gradual improvement of pH is observed which is finally returned to normal values with a concomitant gradual reduction of CO2 tension to the supposed usual level. Oxygen partial pressure remains that expected in a COPD patient in OTLT (figure 5- table 1).
Discussion
Respiratory function is supported by the cooperation between bones and muscles. The skeletal section participates mainly through the movement of the ribs. The contraction of the respiratory muscles combined with the internal and external rotation of the ribs around their axis are the determinants of inspiratory and expiratory movements of the chest wall. In the flail chest a segment of the rib cage is broken in multiple sites detaching from the rest of the chest wall and moving independently from it in the opposite direction during inspiration and expiration, causing a movement that is defined as “paradox” (5, 6). The damage to the bone structure of the thorax induced by rib fractures disrupt the rib cage and substantially affect the respiratory mechanics, causing decreased lung compliance, increased work of breathing, hypoxia an hypoventilation. Particularly dramatic is the case in which these alterations occur in an elderly patient wherein osteoporosis, sarcopenia and comorbidities contribute to decrease the physiological reserves and ability to tolerate the consequences of the traumatic event. In these patients the chest wall is stiffer, the elasticity of the lungs is reduced and systemic vascular resistance increased. Further more, a deterioration of endocrine function with reduced response to trauma and a reduction in glomerular filtration for the urinary excretion of toxic catabolites have been described (7). The paradoxical movement and the presence of pain may determine a shallow breathing with formation of atelectatic areas in the lung parenchyma. The pulmonary contusion in combination with a simultaneous increase in vascular permeability of the pulmonary capillaries in the injured area, leads to extravasation of fluid and the activation of a systemic inflammatory response. The disturbance of diffusion, the reduction in compliance and functional residual capacity and the ventilation-perfusion mismatch create an intrapulmonary shunt with consequent PaO2 reduction and lately PCO2 increase. In addition, the pain resulting from fractures contributes to hypoventilation and prevents expectoration (5). Therefore, respiratory failure in chest trauma is the consequence of the association of pain, atelectasis and pulmonary contusion. NIV prevents airway collapse counteracting the onset of atelectasis, restoring the functional residual capacity and
normalizing the ventilation-perfusion ratio. In our case, the setting of the ventilator followed the necessity to reach a compromise between the aim to obtain
patient’s tolerance to the ventilatory treatment and the fact that she was already suffering of chronic respiratory failure, accepting a moderate level of permissive hypercapnia. Pain management in this patient was also difficult: elderly patients with dementia usually do not adequately express the pain. In this case it was seen that adequately treating pain led to a reduction of accesses of delirium and a better predisposition to ventilatory treatment.
Take home message del caso clinico
• Falls are a frequent cause of multiple trauma in the elderly
• The traumatized elderly patient should be managed taking into account comorbidities and setting a target different from the young patient
• NIV in chest trauma provides a valuable therapeutic option.
References
1. Bollinger CT, Van Eeden FS. Treatment of multiple rib fractures: randomized clinical trial comparing ventilatory with nonventilatory management. Chest 1990 Apr, 97(4): 943-8.
2. Xirouchaki N, Kondoudaki E, Anastasaki M, Alexopoulou C, Koumiotaki S, Georgopoulos D. Noninvasive bilevel positive pressure ventilation in patients with blunt thoracic trauma, Respiration 2005 Sep-Oct, 72(5): 517-22.
3. Hernandez G, Fernandez R, Lopez-Reina P, Cuena R, Pedrosa A, Ortiz R, Hiradier P. Noninvasive ventilation reduces intubation in chest trauma-related hypoxemia; a randomized clinical trial, Chest 2010 Jan, 137(1): 74-80.
4. Gunduz M, Unlugenc H, Ozalevli M, Inanoglu K, Akman H. A comparative study of continuous positive airway pressure (CPAP) and intermittent positive pressure ventilation (IPPV) in patients with flail chest, Emerg Med J. 2005 May, 22(5): 325-9.
5. Pettiford BL, Luketich JD, Landreneau RJ. The management of flail chest. Thorac Surg Clin 2007 Feb;17(1): 25-33.
6. Wanek S, Mayberry JC, Blunt thoracic trauma: flail chest, pulmonary contusion, and blast injury. Crit Care Clin 20 (2004) 71-81.
7. Famà F, Murabito LM, A Beccaria, Cucinotta F, A Caruso, Foti CD, Gioffrè Florio MA. Infuence of co-morbidity in the prognosis of politrauma in geriatric patients BMC Geriatr. 2011;11(Suppl 1): A12.