- Tiziano Pio Valentino
- Original Article
Defining in an objective and simple way the complexity and the severity of an acute patient in the Emergency Medicine Unit: the Complexity-Severity Index (CSI)
- 2/2019-giugno
- ISSN 2532-1285
- https://doi.org/10.23832/ITJEM.2019.016
Tiziano Pio Valentino1 MD, Giulia Cavaliere1 MD, Francesco Pio Cinelli1 MD, Eunice Sofie Cirella2 MD, Raffaella Di Nanno2 MD, Fabrizia Frontuto1 MD, Ettore Procacci3
1) University Polyclinic of Foggia “Ospedali Riuniti”, Department of Emergency Medicine, Foggia, Italy
2) Foggia General Health Institution, Foggia, Italy
3) Student In Medicine and Surgery, University of Foggia, Italy

Abstract
Background
The management of physician workloads in Emergency Medicine could be made on the basis of objective data, improving the procedures and the outcome.
Methods
The aim of this study is to identify the different pathological scenarios in flowcharts in the first anamnestic and diagnostic-therapeutic process and, so, after every change shift in the Emergency Medicine (EM).
The construction of flowcharts is intended to obtain real “numbers”, defined as “COMPLEXITY AND SEVERITY INDEX (CSI)”.
In the period June 2018-February 2019 were collected 210 CSI. The presentation of the same patient was made in two ways to two different physicians during the new shift: the first one explaining it without CSI, the second one by adding the CSI; were recorded in both cases: the time to achieve the understanding of the clinical scenario, moreover, the administration of a simple questionnaire recorded the approval by the doctors, using the CSI, and in the last was recorded the time to obtain the CSI in every patient.
Results
The time necessary to achieve the understanding of the clinical scenario was from 30 seconds to 180 with a mean time of 100 seconds in the group of patients’ folders without CSI, but, in the CSI group the time was from 10 seconds to 150 with a mean time of 70 seconds.
The questionnaire recorded 90% of satisfaction through 20 physicians of the emergency medicine department using CSI added to the patients’ records to simplify the taking care at the change shift.
The time necessary to achieve the CSI, during the recording needed by this study, was from 20 seconds to 90 seconds with a mean time of 30 seconds.
Conclusion
The CSI could improve management the division of workloads, speed up the transfer of patients’ records among emergency doctors, optimizing the outcome.
Keywords
Emergency Medicine; Complexity; Severity; Acute; Index.
Introduction
The Emergency Department, in Italy, changed deeply in about last 10 years: the place where the acute patients find the answer to their health asking is currently also a real admission unit.
The answer to this change is in the reorganization of the number of hospital admission beds by the regional governments by reducing the absolute number.
Moreover the population is more elderly than in the last 20 years and it means that the complexity of the cares is much more than the past.
In Italy the Emergency Departments of the Hub Hospitals or University Teaching Hospitals have a separation between the room/rooms where the patients are visited and treated, and the space where the patients are admitted waiting the end of their diagnostic-therapeutical procedures so called Emergency Medicine Unit.
The importance in the big Hospitals of the Emergency Medicine Unit is evident: in all cases in which in the past the patients with complicated conditions were directly admitted in the medical or cardiological or respiratory Units, the emergency physician can follow and treat, today, all the process of the laboratory and instrumental examinations near his field of work, such as the shock-room.
Moreover, every day the emergency physician are in front of the overcrowding not only outside the visit rooms, but, also in the rooms of the Emergency Medicine Unit.
One of the most crucial moment during the medical shifts is the time of the briefing where the patients not discharged and not admitted in the hospital must be under the care of another doctor working in the Emergency Medicine Unit.
During this process the patients are identified by a subjective way under the point of view of the clinical scenario: for example the geriatric patient with chronic pathologies is considered as a hard patient, even if he or she is only an elderly patient without any acute condition; today, in Emergency Department of the Polyclinic Foggia, the moment of the medical shift is linked to the emotivity of the physicians; the most important thing is the total number of the patients that must be take in charge by the physician of the Emergency Medicine Unit: the real clinical situation is secondary respect the total “number” of patients.
The aim of this observational study is to identify a “number” assigned to every patient before every change of physicians’ work shift; the “number” can gather in a simple way all the clinical conditions of the patient at the time of the admission in the Emergency Department and it can be change during the staying in the Emergency Medicine Unit.
In the literature there are not works concerning the building of this Index, so we propose a new approach to see in an objective way the clinical scenario of the Emergency Medicine Unit patients.
Byrne et al.1 defined the relationship of the clinical acuity and complexity to the outcome of an emergency medical admission, stating that the Risk Score was age related and strongest outcome determinant was Acute Illness Severity.
Nannan Panday et al.2 shows the prognostic value of early warning scores in the emergency department and acute medical unit, reviewing the literature, but this work was useful just to achieve a rationale in the prognosis assigning of the admitted patients.
Methods
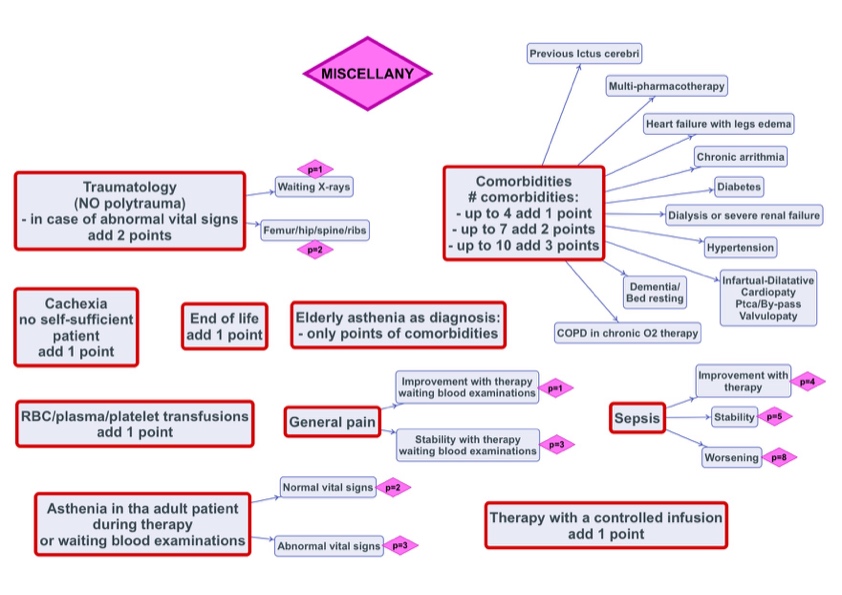
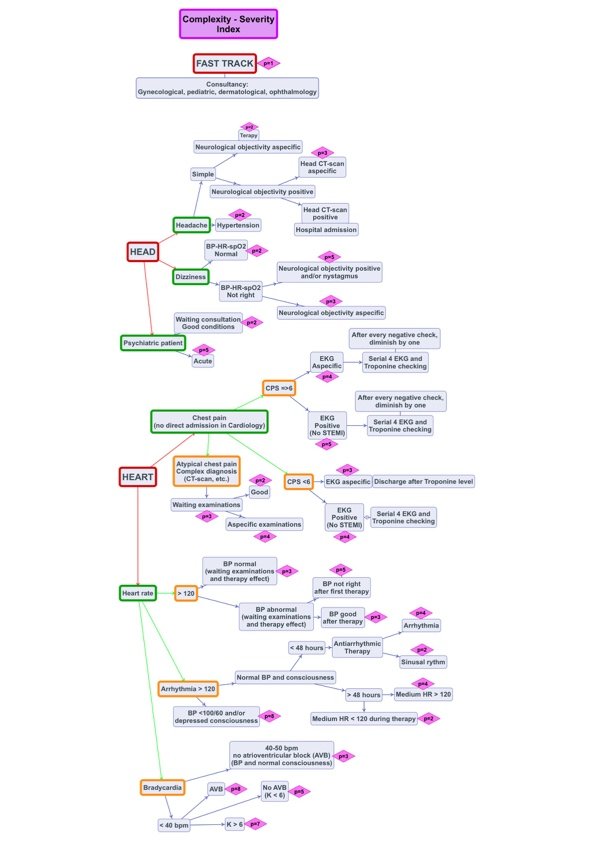
The Complexity-Severity-Index (CSI) can be built by following ad-hoc flow-charts for every pathological or simply not-right condition (Figure 1-5): in fact in the Emergency Department often can be seen people that need just of something to eat or a place where to sleep in the winter season, without any acute pathological condition.
In addiction to the first obtained number, we added another 4 numbers (Figure 1):
- a number derived from the total number of co-morbidity ;
- one number linked to eventual intra-venous controlled speed therapy ;
- one number derived from actual blood/platelet/plasma transfusions ;
- actual condition of obliged bed rest in elderly or oncologic or not autonomous patients;
Figure 1
Figure 2
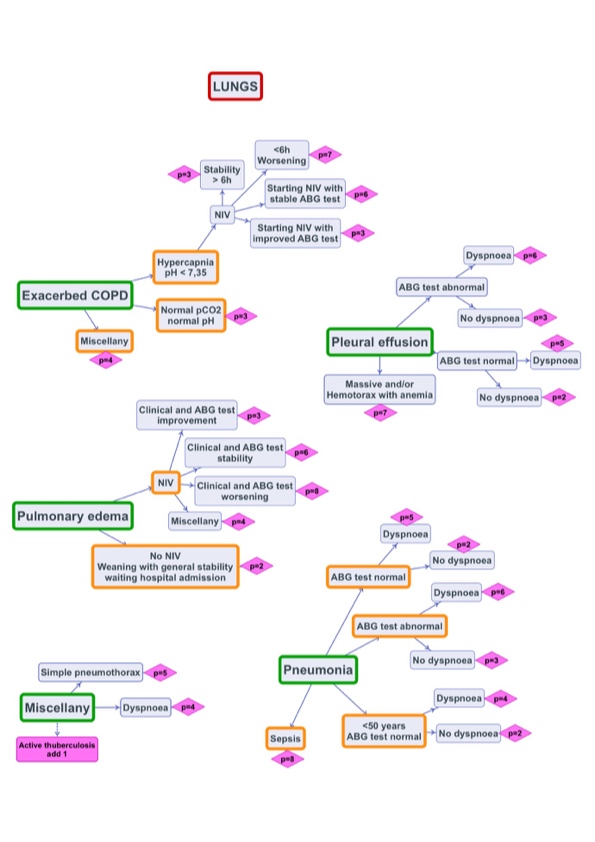
Figure 3
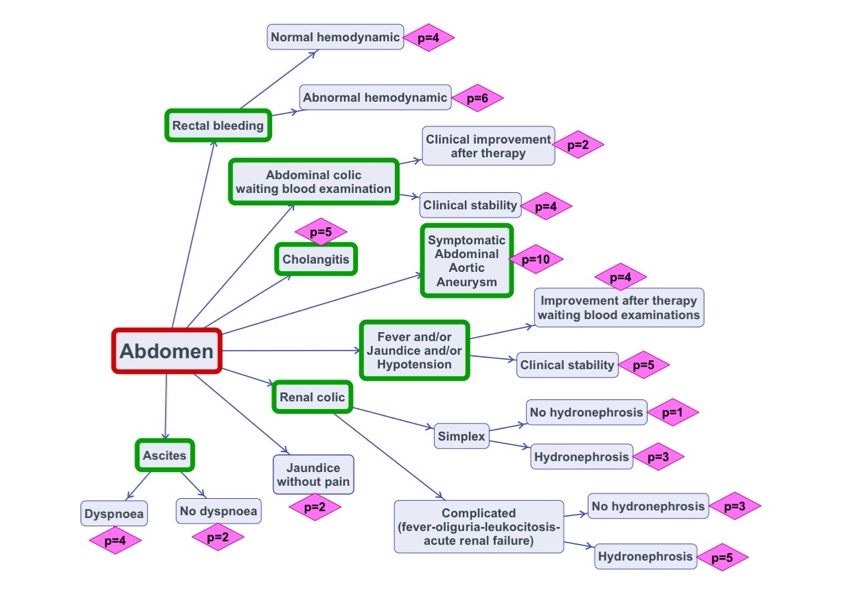
Figure 4
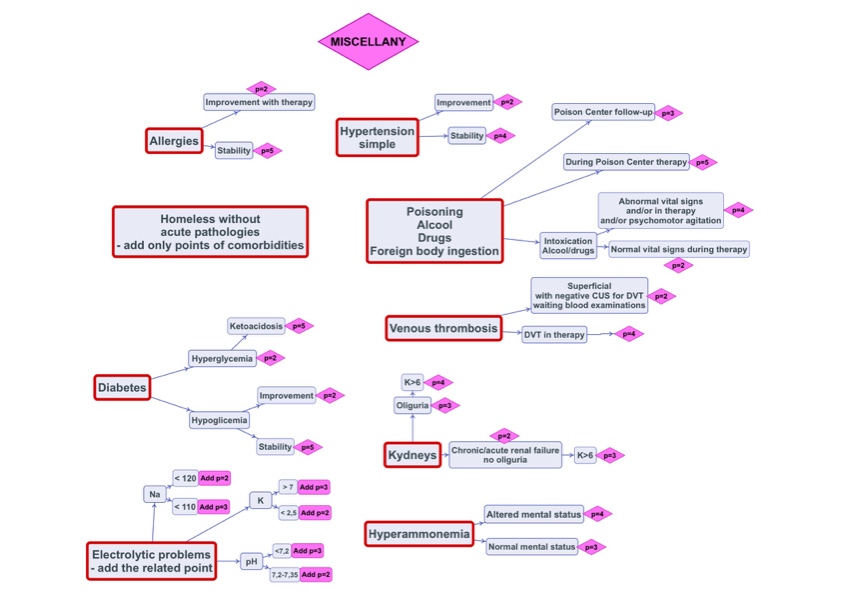
Figure 5
The sum of these 4 numbers must be reduced by the number of the days of staying of the patient in the Emergency Medicine Unit: the rationale of this fact, in the most part of cases, is that more days the patient is in the Emergency Medicine Unit, better is the diagnostic evaluation and the therapeutic course; moreover the time limit of the stay of a patient in the Emergency Medicine Unit (EMU) is no more 72 hours. In the period from June 2018 to February 2019 were collected 210 CSI, built by the above mentioned process.
The presentation of the same clinical case in the EMU was conducted in two ways: two different physicians during the new shift had the same patient; the first one received the case explaining it thoroughly by talking about all the clinical conditions in a subjective way; the second one had, also, the indication of the calculated CSI together with a brief classical explanation of the clinical scenario.
A satisfaction form was given to every physician in every new shift working in the EMU to collect the satisfaction derived by the use of the CSI.
The total time necessary to give-receive the clinical case was collected together with the time necessary to build the CSI at the admission and during every shift.
The flow-charts were built on the basis of diagnostic paths of current use into the Emergency Department of the Polyclinic of Foggia, initially setting a cut-off limit greater than or equal to 6 to describe a clinical case of greater severity and complexity; during the data collection, the number of 6 was considered adherent to what were the real management times of a critical patient from the point of view of the complexity of diagnosis and treatment. The data were collected by trainees graduated in medicine and surgery and by a student in medicine and surgery; the satisfaction questionnaires were administered by the first author to the doctors in the EMU, as well as the detection of all times.
Results
The time necessary to achieve the understanding of the clinical scenario was from 30 seconds to 180 with a mean time of 100 seconds in the group of patients’ folders without CSI, but, in the CGI group the time was from 10 seconds to 150 with a mean time of 70 seconds.
The questionnaire recorded 90% of satisfaction through 20 physicians of the EMU using CSI added to the patients’ records to simplify the taking care at the change shift.
The time necessary to achieve the CSI, during the recording needed by this study, was from 20 seconds to 90 seconds with a mean time of 30 seconds.
Discussion - Conclusion
The use of CSI has proved useful, in our experience, to speed up the mechanism of delivery of medical records of patients admitted to emergency medicine, during the shift period, rationalizing the number of patients to be assigned to each doctor, based on the complexity of diagnosis and therapy; even if on the basis of a few cases considered in this study, the use of CSI could be a quick and easy application for all patients involved in an Emergency Medicine Unit, to improve the management of all patients left in the next work shift, making every clinical case with an absolute number from the point of view of clinical complexity and severity.
References
- Byrne D, Conway R, Cournane S, O’Riordan D, Silke B. Relationship of the clinical acuity & complexity to the outcome of an emergency medical admission. Acute Med. 2018; 17(1):18- 25.
- Nannan Panday RS, Minderhoud TC, Alam N, Nanayakkara PWB. Prognostic value of early warning scores in the emergency department (ED) and acute medical unit (AMU): A narrative review. Eur J Intern Med. 2017 Nov; 45:20-31.